Implant Surgery Complications: Risk Factors and Prevention Strategies
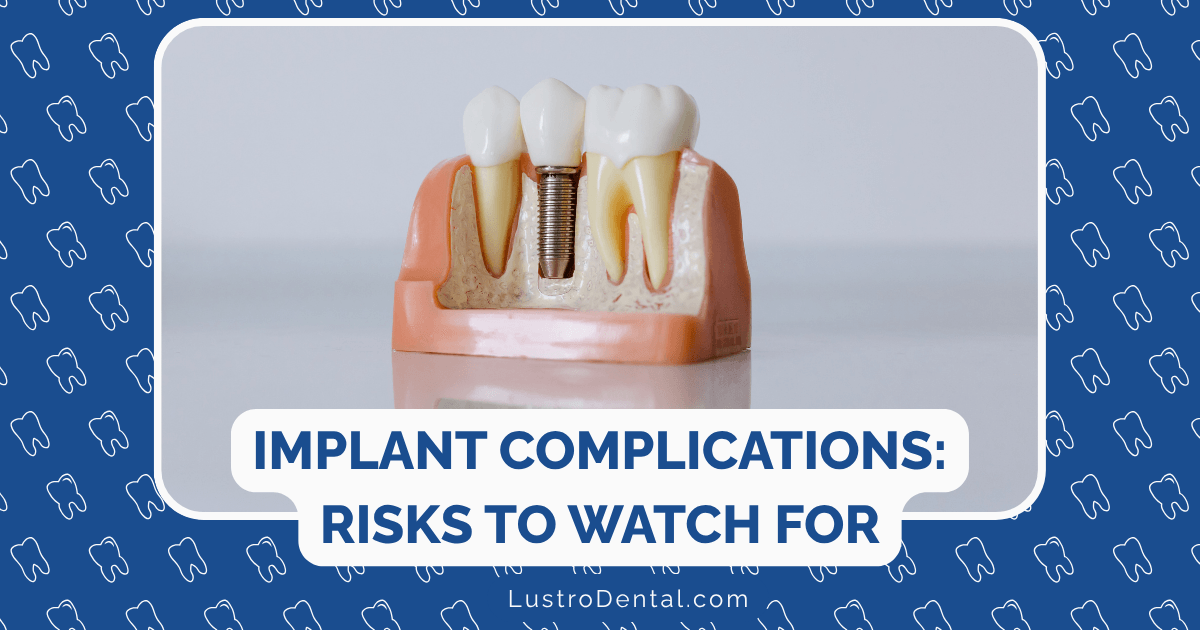
Dental implants have revolutionized tooth replacement, offering a solution that closely mimics natural teeth in both function and appearance. With success rates typically above 95%, they’re one of the most predictable procedures in modern dentistry. However, like any surgical procedure, implant placement isn’t without risks.
As someone who’s guided many patients through their implant journeys, I believe that understanding potential complications—and how to prevent them—is essential for making informed decisions about your dental care. Knowledge isn’t meant to frighten but to empower, allowing you to take proactive steps toward a successful outcome.
In this comprehensive guide, we’ll explore the most common implant complications, identify key risk factors, and outline evidence-based strategies to minimize these risks at every stage of your implant journey.
Understanding Implant Success and Failure
Before diving into complications, let’s clarify what constitutes implant success versus failure:
Implant Success is typically defined as:
- An implant that’s firmly anchored in bone (osseointegrated)
- Free from infection and inflammation
- Supporting its prosthetic tooth effectively
- Comfortable and functional
- Maintaining stable bone levels long-term
Implant Failure can be categorized as:
- Early failure: Occurs before osseointegration is complete (typically within the first few months)
- Late failure: Develops after the implant has initially integrated successfully
According to a 2022 study published in the Journal of Oral and Maxillofacial Surgery, the overall implant failure rate is approximately 3.11%, with late failures (75%) being more common than early failures (25%).
Common Implant Complications: What Can Go Wrong
Complications can be divided into early (occurring during or shortly after surgery) and late (developing months or years later) categories:
Early Complications
1. Infection
Bacterial contamination during or after surgery can lead to infection, characterized by pain, swelling, redness, and sometimes discharge.
2. Nerve Injury
The surgical placement of implants, particularly in the lower jaw, can potentially damage nerves, resulting in numbness, tingling, or pain in the lips, chin, tongue, or surrounding tissues.
3. Sinus Problems
Upper jaw implants placed too close to or penetrating the sinus cavity can cause sinusitis or other sinus-related issues.
4. Excessive Bleeding
While some bleeding is normal after surgery, excessive or prolonged bleeding may indicate a complication.
5. Failed Initial Integration
Sometimes the implant fails to properly fuse with the surrounding bone during the initial healing phase.
Late Complications
1. Peri-implantitis
This inflammatory condition affects the soft and hard tissues surrounding a dental implant, leading to progressive bone loss and potentially implant failure if left untreated.
According to a meta-analysis published in Clinical Oral Investigations, peri-implantitis affects approximately 13% of implants and 18.5% of patients, with rates rising from 0.4% to 43.9% within 3-5 years.
2. Mechanical Complications
These include:
- Loose or fractured abutment screws
- Fractured implants
- Broken prosthetic components
3. Aesthetic Complications
Issues with the appearance of the implant restoration, such as:
- Visible metal margins
- Gum recession
- Improper crown contours
4. Progressive Bone Loss
Gradual loss of bone around an implant beyond what’s considered normal.
Risk Factors: Who’s Most Vulnerable to Complications?
Understanding risk factors is crucial for prevention. These can be divided into patient-related and procedure-related factors:
Patient-Related Risk Factors
1. Periodontal Disease History
Research from the International Team for Implantology shows that patients with a history of periodontitis have a 2.21 times higher risk of developing peri-implantitis. A 10-year study found peri-implantitis in 29% of patients with previous periodontal disease compared to just 6% in those without.
2. Smoking
Tobacco use significantly impairs healing and increases complication rates. A meta-analysis found that smokers have approximately double the risk of implant failure compared to non-smokers, with a relative risk of 2.07 (95% CI 1.41, 3.04).
Dr. Sarah Johnson, an implantologist at Mayo Clinic, emphasizes: “Smoking is perhaps the most significant modifiable risk factor for implant complications. The chemicals in tobacco impair blood flow to the surgical site, inhibit healing, and increase infection risk.”
3. Uncontrolled Diabetes
Poorly controlled diabetes impairs healing and increases infection risk. Research shows that individuals with poorly controlled diabetes have a 46% higher risk of developing peri-implantitis compared to those with normal blood glucose levels.
4. Poor Oral Hygiene
Inadequate plaque control is strongly associated with peri-implantitis and implant failure.
5. Bruxism (Teeth Grinding)
Excessive forces from grinding or clenching can lead to mechanical complications and bone loss around implants.
6. Certain Medications
Some medications, including high-dose bisphosphonates and immunosuppressants, can affect implant healing and integration.
7. Systemic Conditions
Autoimmune disorders, uncontrolled cardiovascular disease, and other systemic conditions may impact healing and long-term implant success.
8. Genetic Factors
Research has identified certain genetic markers associated with increased peri-implantitis risk. For example, IL-1 polymorphisms have been linked to a 1.9 to 2.47 times higher risk, while TNF-α polymorphism has been associated with a five to eightfold increased risk.
Procedure-Related Risk Factors
1. Inadequate Bone Quantity/Quality
Insufficient bone volume or density significantly increases failure risk. According to the Journal of Oral and Maxillofacial Surgery study, type III-IV (soft) bone density was found in 75% of failed implants.
2. Improper Implant Positioning
Implants placed too close to vital structures, adjacent teeth, or in poor angulation have higher complication rates.
3. Inadequate Keratinized Tissue
Less than 2mm of keratinized (firm) gum tissue around implants is associated with increased inflammation and complications.
4. Overheating During Surgery
Excessive heat generation during implant site preparation can damage bone cells and impair osseointegration.
5. Excessive Surgical Trauma
Traumatic surgical technique can compromise healing and integration.
6. Immediate Loading Without Adequate Primary Stability
Placing functional forces on implants too early without sufficient initial stability can lead to micromotion and failure.
7. Retained Cement
Excess cement from crown cementation can cause peri-implant inflammation and tissue damage.
Prevention Strategies: Minimizing Your Risk
Prevention strategies should address both patient-related and procedure-related risk factors at every stage of the implant process:
Before Surgery: Preparation Phase
1. Comprehensive Assessment and Planning
- 3D imaging (CBCT scans) to evaluate bone quality, quantity, and proximity to vital structures
- Thorough medical history review to identify systemic risk factors
- Periodontal evaluation and treatment of any existing gum disease
- Smoking cessation at least 2 weeks before surgery (longer is better)
- Blood glucose control for diabetic patients
Dr. Michael Chen of Dynamic Dental notes, “The most successful implant cases begin with meticulous planning. Using 3D imaging and surgical guides significantly reduces the risk of nerve damage and improper positioning.”
2. Optimize Oral Health
- Professional cleaning to reduce bacterial load
- Treatment of active infections before implant placement
- Oral hygiene instruction to establish good habits
3. Address Modifiable Risk Factors
- Smoking cessation programs and support
- Nutritional counseling to optimize healing
- Management of parafunctional habits (night guard for bruxism)
- Medication review with your physician if you’re taking drugs that might affect healing
During Surgery: Procedural Strategies
1. Strict Aseptic Technique
- Sterile surgical environment
- Proper draping and isolation
- Antibacterial mouth rinse before surgery
2. Atraumatic Surgical Technique
- Gentle tissue handling
- Adequate cooling during drilling
- Appropriate drill sequence
3. Proper Implant Selection and Positioning
- Appropriate implant size and design for the site
- Optimal three-dimensional positioning
- Safe distance from vital structures
4. Consider Guided Surgery
Computer-guided implant placement using surgical guides can significantly improve accuracy and reduce complications.
5. Prophylactic Measures
- Preoperative antibiotics for high-risk patients
- Anti-inflammatory medications to manage swelling
After Surgery: Recovery and Maintenance
1. Immediate Post-Operative Care
- Follow all post-operative instructions
- Take prescribed medications as directed
- Apply ice to minimize swelling
- Maintain a soft diet during initial healing
- Avoid smoking and alcohol
2. Establish Proper Oral Hygiene
- Gentle cleaning around the implant site
- Use of recommended oral hygiene aids (water flossers, interdental brushes)
- Antibacterial mouth rinses if prescribed
3. Regular Maintenance Visits
The importance of professional maintenance cannot be overstated. According to research in Clinical Oral Investigations, patients who don’t comply with maintenance therapy have a 20% chance of developing peri-implantitis within 5 years, while compliance is associated with an 86% reduction in peri-implantitis cases.
A typical maintenance schedule includes:
- 3-4 month professional cleanings for high-risk patients
- 6-month cleanings for standard-risk patients
- Annual radiographs to monitor bone levels
- Regular evaluation of implant stability and function
4. Long-Term Risk Management
- Ongoing management of systemic conditions like diabetes
- Continued abstinence from smoking
- Night guard use for patients with bruxism
- Prompt attention to any warning signs
Warning Signs: When to Seek Help
Early intervention is crucial when complications arise. Contact your dentist immediately if you notice:
- Pain or discomfort that persists or worsens after the initial healing period
- Swelling that develops or increases after the first few days
- Bleeding that continues beyond the first day
- Implant mobility or a feeling that the implant is loose
- Pus or discharge around the implant
- Unpleasant taste or odor from the implant area
- Receding gums around the implant
- Visible metal at the gum line
- Difficulty chewing or discomfort when biting
Treatment Approaches for Complications
If complications do occur, various treatment approaches are available:
For Peri-implantitis
- Non-surgical therapy: Professional cleaning, local antimicrobials, oral hygiene instruction
- Surgical therapy: Open flap debridement, regenerative procedures
- Implant surface decontamination: Mechanical, chemical, or laser treatments
For Mechanical Complications
- Retightening or replacing loose components
- Occlusal adjustment to reduce excessive forces
- Night guard fabrication for bruxism protection
For Aesthetic Complications
- Soft tissue grafting for recession
- Prosthetic modifications or replacement
For Failed Implants
- Removal of the failed implant
- Site preservation with bone grafting
- Consideration of alternative treatment options or re-implantation after healing
The Reality of Implant Complications: Keeping Perspective
While understanding complications is important, it’s equally important to maintain perspective. With proper patient selection, planning, surgical technique, and maintenance, dental implants remain one of the most successful and predictable procedures in dentistry.
Dr. Lisa Wong of Springfield Perio & Implants reminds us, “The vast majority of dental implant patients enjoy decades of trouble-free function. When complications do occur, most can be effectively managed, especially when caught early.”
Final Thoughts: A Proactive Approach to Implant Success
Dental implant complications, while relatively rare, can significantly impact your oral health and quality of life. By understanding risk factors and implementing prevention strategies, you can dramatically reduce your chances of experiencing problems.
The key takeaways for implant success include:
- Honest communication with your dental provider about your medical history and risk factors
- Addressing modifiable risk factors before surgery (especially smoking and periodontal disease)
- Choosing an experienced implant surgeon with advanced training
- Following all pre- and post-operative instructions carefully
- Maintaining impeccable oral hygiene around your implants
- Committing to regular professional maintenance and monitoring
- Seeking prompt attention for any concerning symptoms
With this proactive approach, you can maximize your chances of enjoying the life-changing benefits of dental implants for many years to come.
Have you had dental implant surgery or are you considering it? What concerns do you have about potential complications? Share your thoughts or questions in the comments below to help others on their implant journey.