Chronic Dry Mouth: Causes Beyond the Obvious
That persistent feeling of cotton mouth. The constant need to sip water. The discomfort that makes speaking and eating challenging. If you’re experiencing these symptoms regularly, you’re likely dealing with chronic dry mouth, or what medical professionals call xerostomia.
While many people associate dry mouth primarily with medication side effects (and rightfully so—they are indeed the most common cause), there’s a whole universe of less obvious factors that could be leaving you parched. As a dental health advocate dedicated to helping people understand and address their oral health concerns, I’ve encountered numerous patients struggling with this condition without understanding its true origin.
Understanding Xerostomia: More Than Just Thirst
Xerostomia affects approximately one in five people, with prevalence increasing with age. It’s not merely an inconvenience—chronic dry mouth can significantly impact your quality of life and oral health.
When your salivary glands don’t produce enough saliva, you lose more than just moisture. Saliva plays crucial roles in:
- Neutralizing acids produced by bacteria
- Washing away food particles
- Remineralizing teeth
- Facilitating taste and digestion
- Fighting germs that cause bad breath and infection
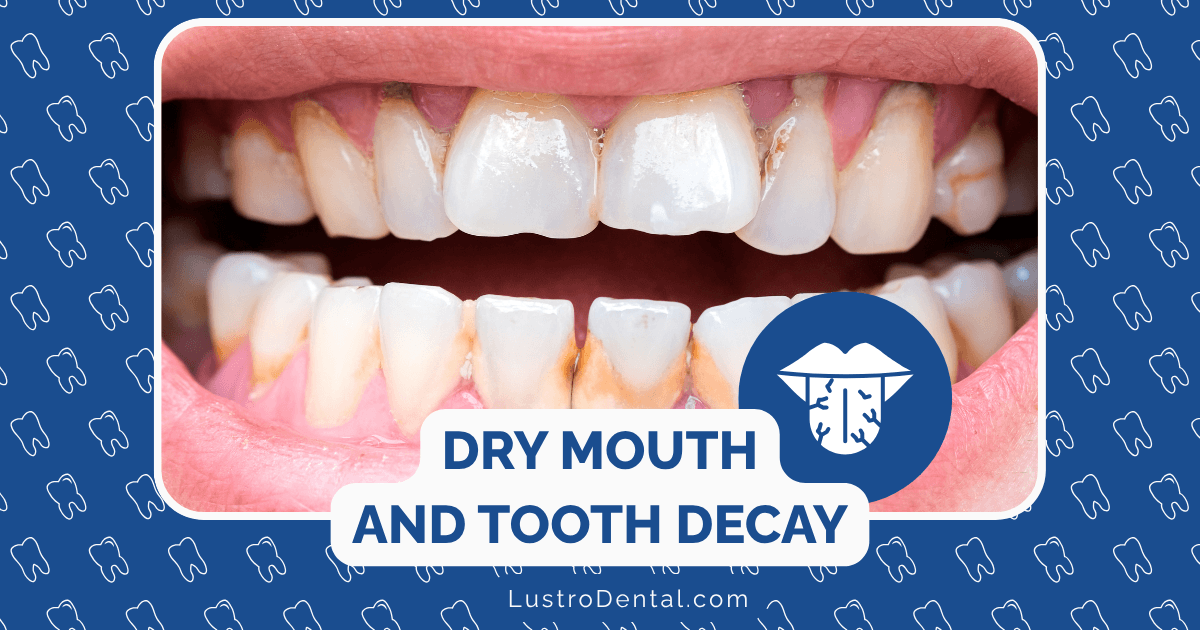
Without adequate saliva, your risk of tooth decay, gum disease, and oral infections increases dramatically. That’s why identifying the true cause of your dry mouth is essential for effective treatment.
The Well-Known Culprits: A Brief Recap
Before diving into the less obvious causes, let’s quickly acknowledge the common suspects:
- Medications: Over 500 medications list dry mouth as a side effect, including antihistamines, antidepressants, antihypertensives, and diuretics.
- Dehydration: Not consuming enough fluids can naturally reduce saliva production.
- Aging: The natural aging process can affect salivary gland function.
But what if you’ve ruled these out and are still suffering? Let’s explore the less obvious causes that might be behind your chronic dry mouth.
Beyond the Obvious: Unexpected Causes of Chronic Dry Mouth
1. Autoimmune Disorders Beyond Sjögren’s Syndrome
While Sjögren’s syndrome is the most well-known autoimmune condition associated with dry mouth, several other autoimmune disorders can affect salivary function:
- Systemic Lupus Erythematosus (SLE): This chronic autoimmune disease can attack various body systems, including the salivary glands.
- Rheumatoid Arthritis: Beyond joint inflammation, RA can affect exocrine glands.
- Thyroid Disorders: Both hypothyroidism and hyperthyroidism can contribute to dry mouth symptoms.
- Primary Biliary Cirrhosis (PBC): This progressive liver disease often presents with dry mouth as an early symptom.
These conditions typically require diagnosis by a rheumatologist or specialist, so if you have unexplained dry mouth alongside other systemic symptoms, consider requesting appropriate testing.
2. Neurological Conditions and Nerve Damage
Your salivary glands rely on proper nerve signaling to function correctly. Damage to or conditions affecting these nerve pathways can result in reduced saliva production:
- Bell’s Palsy: This temporary facial paralysis can affect the nerves controlling salivation.
- Stroke: Depending on the affected brain area, stroke survivors may experience dry mouth.
- Nerve Damage from Surgery or Trauma: Injuries to the head and neck region can disrupt the neural pathways to salivary glands.
- Parkinson’s Disease: Autonomic dysfunction in Parkinson’s can affect saliva production and swallowing.
A 2023 study published in the Journal of Oral Rehabilitation found that nearly 60% of patients with certain types of nerve damage reported chronic dry mouth symptoms, highlighting this often-overlooked connection.
3. Sleep-Related Factors
Your sleeping habits might be contributing to your dry mouth more than you realize:
- Mouth Breathing: Whether due to nasal congestion, anatomical factors, or habit, breathing through your mouth during sleep dramatically increases oral dryness.
- Sleep Apnea: This common sleep disorder often leads to mouth breathing and dry mouth. The use of CPAP machines, while beneficial for sleep apnea, can sometimes exacerbate dry mouth symptoms.
- Nighttime Dehydration: If you’re not adequately hydrated before bed or sleep in a very dry environment, you may wake with significant dry mouth.
Consider a sleep study if you suspect sleep-related breathing issues may be contributing to your symptoms.
4. Endocrine and Metabolic Disorders
Several metabolic conditions can contribute to xerostomia:
- Uncontrolled Diabetes: High blood sugar levels can lead to dehydration and reduced saliva production. According to the American Diabetes Association, dry mouth is a common complaint among diabetic patients, particularly those with uncontrolled blood glucose.
- Thyroid Dysfunction: Both hypothyroidism and hyperthyroidism can affect salivary gland function.
- Adrenal Insufficiency: Conditions like Addison’s disease that affect hormone production can impact fluid balance throughout the body, including saliva.
Regular monitoring of these conditions and working with your healthcare provider to maintain optimal control can help reduce dry mouth symptoms.
5. Chronic Stress and Anxiety
The mind-body connection is powerful, and psychological factors can significantly impact your physical symptoms:
- Chronic Stress: Prolonged stress activates the sympathetic nervous system (fight-or-flight response), which can reduce salivary flow.
- Anxiety Disorders: Anxiety can cause mouth breathing, altered autonomic nervous system function, and reduced saliva production.
- Depression: Both the condition itself and many antidepressant medications can contribute to dry mouth.
Incorporating stress management techniques like mindfulness, meditation, or cognitive behavioral therapy may help alleviate these symptoms alongside other treatments.
6. Nutritional Deficiencies and Dietary Factors
What you eat—or don’t eat—can influence your oral moisture levels:
- Vitamin B Deficiencies: Particularly B12 and folate, which are important for cellular function, including in salivary glands.
- Iron Deficiency: Can affect tissue health throughout the body, including oral tissues.
- Dehydrating Foods and Beverages: Excessive consumption of caffeine, alcohol, and salty or spicy foods can contribute to dry mouth.
- Acidic Diet: Regularly consuming highly acidic foods and beverages can alter oral pH and affect saliva quality.
A balanced diet rich in vitamins and minerals, along with adequate hydration, supports optimal salivary gland function.
7. Environmental Factors
Your surroundings may be contributing to your dry mouth:
- Low Humidity: Dry indoor air, especially in winter or in air-conditioned environments, can increase oral dryness.
- Pollutants and Irritants: Exposure to certain chemicals, smoke, or pollutants can irritate oral tissues and affect saliva production.
- High Altitudes: The lower oxygen levels and typically drier air at high elevations can exacerbate dry mouth symptoms.
Using a humidifier, especially while sleeping, can help maintain optimal moisture levels in your environment.
8. Radiation Exposure
While most people associate radiation-induced dry mouth with cancer treatments, other less obvious sources of radiation exposure can affect salivary function:
- Previous Radiation Therapy: Even radiation treatment that occurred years ago can have lasting effects on salivary glands.
- Radioactive Iodine Treatment: Used for thyroid conditions, this can sometimes affect salivary gland function.
- Certain Diagnostic Procedures: Some specialized imaging techniques may temporarily affect salivation.
According to research from the National Institute of Dental and Craniofacial Research, salivary glands are particularly sensitive to radiation, with effects potentially lasting long after exposure.
9. Chronic Infections
Certain infections can directly or indirectly affect salivary gland function:
- HIV/AIDS: Salivary gland disease is common among people living with HIV.
- Hepatitis C: Can cause sialadenitis (salivary gland inflammation).
- Bacterial Sialadenitis: Bacterial infections of the salivary glands can lead to reduced function.
- Mumps: While less common today due to vaccination, mumps virus specifically targets salivary glands.
Proper diagnosis and treatment of these underlying infections is essential for addressing related dry mouth symptoms.
10. Genetic Factors
Some people may have a genetic predisposition to salivary gland dysfunction:
- Congenital Salivary Gland Disorders: Some individuals are born with underdeveloped or dysfunctional salivary glands.
- Genetic Conditions: Certain rare genetic disorders can affect exocrine gland function, including salivary glands.
- Family History: A family history of autoimmune disorders affecting salivary function may increase your risk.
Genetic testing and consultation with specialists may be appropriate if other causes have been ruled out.
Diagnosing the True Cause of Your Chronic Dry Mouth
If you’re experiencing persistent dry mouth, a systematic approach to diagnosis is essential:
- Comprehensive Medical History: Be sure to discuss all medications (prescription and over-the-counter), medical conditions, and lifestyle factors with your healthcare provider.
- Physical Examination: A thorough examination of your mouth, salivary glands, and overall health can provide important clues.
- Salivary Flow Testing: Simple tests can measure your saliva production to determine the severity of your condition.
- Blood Tests: These can identify autoimmune markers, nutritional deficiencies, or signs of systemic conditions.
- Imaging Studies: In some cases, ultrasound, MRI, or CT scans of the salivary glands may be necessary.
- Salivary Gland Biopsy: In rare cases, a small tissue sample may be needed to make a definitive diagnosis.
- Specialist Referrals: Depending on findings, you may be referred to specialists such as rheumatologists, neurologists, or otolaryngologists.
Managing Chronic Dry Mouth: A Holistic Approach
Once you’ve identified the underlying cause of your dry mouth, targeted treatment can begin. However, regardless of the cause, these strategies can help manage symptoms:
Daily Management Strategies
- Stay Hydrated: Sip water throughout the day and keep water by your bedside at night.
- Use Sugar-Free Lozenges or Gum: These stimulate saliva flow without increasing cavity risk.
- Try Alcohol-Free Mouthwash: Specifically formulated for dry mouth, these can provide temporary relief.
- Consider a Humidifier: Especially while sleeping to maintain optimal environmental moisture.
- Avoid Irritants: Minimize consumption of alcohol, caffeine, tobacco, and spicy or acidic foods.
- Practice Good Oral Hygiene: Brush twice daily with fluoride toothpaste, floss daily, and see your dentist regularly.
Advanced Treatment Options
- Saliva Substitutes: Available as sprays, gels, or lozenges, these can provide longer-lasting relief than water.
- Prescription Medications: Salivary stimulants like pilocarpine (Salagen) or cevimeline (Evoxac) may be prescribed for certain conditions.
- Acupuncture: Some studies suggest acupuncture may help stimulate salivary flow in certain patients.
- Transcutaneous Electrical Nerve Stimulation (TENS): This therapy may help stimulate salivary glands in some cases.
- Addressing Underlying Conditions: Working with specialists to optimally manage any contributing health conditions.
When to Seek Professional Help
While occasional dry mouth is normal, you should consult a healthcare provider if you experience:
- Persistent dry mouth lasting more than two weeks
- Dry mouth accompanied by other symptoms like joint pain, fatigue, or vision changes
- Difficulty eating, speaking, or swallowing due to dry mouth
- Noticeable changes in the appearance of your tongue or oral tissues
- Increased tooth decay despite good oral hygiene
The Future of Dry Mouth Treatment
Research into xerostomia treatment continues to advance. Promising developments include:
- Gene Therapy: Research is underway on transferring aquaporin genes to increase fluid secretion in damaged salivary glands.
- Stem Cell Therapy: The MARSH clinical trial is investigating stem cell regenerative therapy for radiation-induced xerostomia.
- Artificial Salivary Glands: Bioengineering research aims to develop implantable artificial salivary glands for severe cases.
- Targeted Drug Delivery: New methods to deliver medications directly to salivary glands with fewer systemic side effects.
Conclusion: Finding Relief Through Understanding
Chronic dry mouth is more than just an annoyance—it’s a condition that can significantly impact your oral health and quality of life. By looking beyond the obvious causes and considering these less common factors, you and your healthcare providers can better identify the true source of your symptoms and develop an effective treatment plan.
Remember that xerostomia often requires a multidisciplinary approach. Your dentist, primary care physician, and potentially other specialists may all play important roles in diagnosis and treatment. Don’t hesitate to advocate for yourself and seek the care you need to find relief from this challenging condition.
Have you discovered an unexpected cause behind your dry mouth symptoms? Share your experience in the comments below to help others who might be facing similar challenges.