Sleep Apnea and Dentistry: How Oral Appliances Can Help You Breathe Better
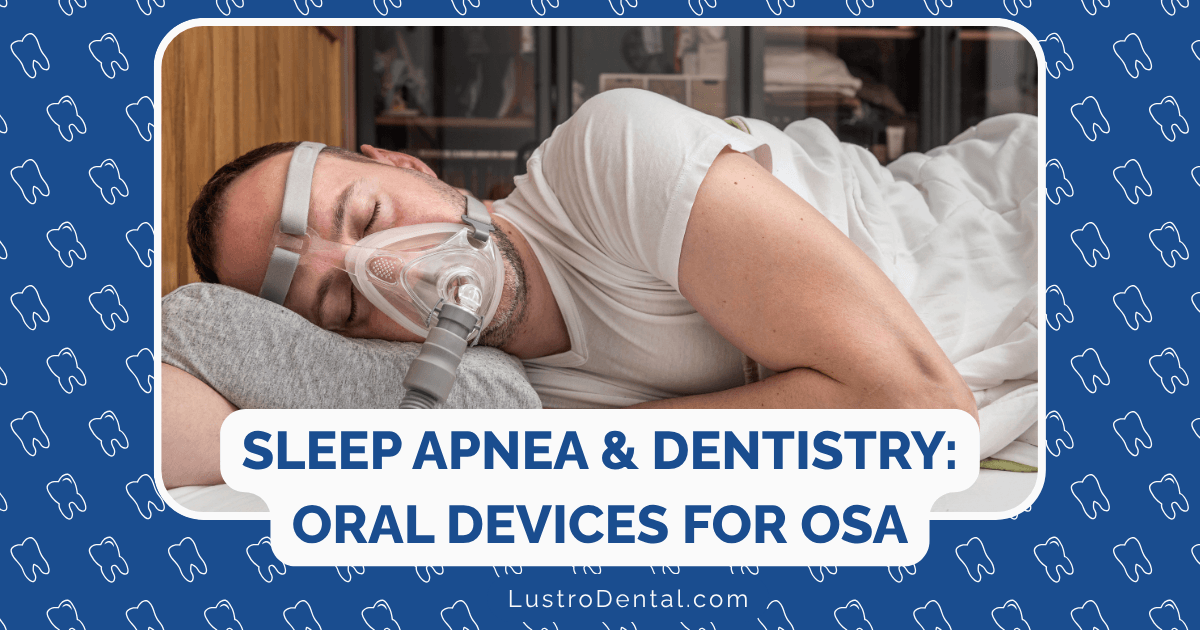
The sound of silence should be golden, especially at night. Yet for millions of people suffering from obstructive sleep apnea (OSA), nighttime brings a symphony of snoring, gasping, and breathing interruptions that disrupt not only their sleep but often their partner’s as well. Beyond the noise lies a serious health concern: repeatedly stopped breathing during sleep that can lead to significant health complications if left untreated.
As a dental health advocate, I’ve witnessed how this common sleep disorder affects not just physical health but quality of life. While Continuous Positive Airway Pressure (CPAP) therapy has long been considered the gold standard treatment, many patients struggle with its use. This is where modern dentistry offers a valuable alternative: oral appliance therapy.
In this comprehensive guide, we’ll explore how dental solutions for sleep apnea work, their effectiveness compared to other treatments, and how they might be the breathing solution you’ve been searching for.
Understanding Sleep Apnea: More Than Just Snoring
Before diving into dental solutions, it’s important to understand exactly what we’re treating. Obstructive sleep apnea occurs when the muscles in the back of your throat relax too much during sleep, allowing soft tissue to collapse and block your airway. This blockage causes breathing to stop temporarily—from a few seconds to over a minute—before your brain signals your body to restart breathing, often with a gasp or choking sound.
These episodes can occur 5-30 times (or more) per hour throughout the night, preventing restorative deep sleep and reducing oxygen levels in your blood. The consequences extend far beyond feeling tired the next day.
Health Implications of Untreated Sleep Apnea
Research has linked untreated sleep apnea to numerous serious health conditions:
- Cardiovascular problems: Increased risk of high blood pressure, heart attack, stroke, and irregular heartbeats
- Metabolic issues: Greater likelihood of developing type 2 diabetes and metabolic syndrome
- Cognitive impairment: Memory problems, difficulty concentrating, and increased risk of accidents
- Mental health concerns: Higher rates of depression and anxiety
- Liver complications: Greater risk of nonalcoholic fatty liver disease
- Sleep deprivation: Chronic fatigue, daytime sleepiness, and reduced quality of life
Dr. Sarah Johnson, a sleep medicine specialist, explains: “Many patients don’t realize that their snoring, morning headaches, or daytime fatigue could indicate a serious condition. The intermittent oxygen deprivation associated with sleep apnea puts tremendous stress on virtually every system in the body.”
The Dental Connection: How Your Mouth Affects Your Breathing
The relationship between dentistry and sleep breathing disorders is more significant than many realize. Certain oral and facial characteristics can predispose individuals to sleep apnea:
- Retrognathia: A recessed lower jaw that narrows the airway
- Macroglossia: An enlarged tongue that can fall back during sleep
- High, narrow palate: Creates less room for nasal breathing
- Tonsil and adenoid enlargement: Narrows the airway passage
- Deviated septum: Restricts nasal airflow, increasing mouth breathing
Dentists are uniquely positioned to identify these risk factors during routine examinations. In fact, a 2025 study published in Nature found that dental professionals can play a crucial role in both screening for and treating sleep-disordered breathing.
Oral Appliance Therapy: A Dental Solution for Better Breathing
Oral appliance therapy involves wearing a custom-fitted device in your mouth during sleep. These devices work by repositioning oral structures to maintain an open airway throughout the night.
How Oral Appliances Work
Depending on the specific type, oral appliances function through one or more of these mechanisms:
- Repositioning the lower jaw: Moving the mandible (lower jaw) forward pulls the tongue away from the back of the throat, preventing airway collapse.
- Stabilizing the tongue: Some devices hold the tongue in a forward position to keep the airway clear.
- Increasing muscle tone: Certain appliances help activate and tone the muscles that keep the airway open.
According to research published by the American Academy of Dental Sleep Medicine, these devices can significantly reduce the severity of sleep apnea and associated symptoms in many patients.
Types of Oral Appliances
Several types of oral appliances are available, each with specific benefits and considerations:
1. Mandibular Advancement Devices (MADs)
The most common type of oral appliance for sleep apnea, MADs look similar to sports mouthguards but with a crucial difference: they’re designed to hold the lower jaw slightly forward. This forward positioning helps keep the airway open by preventing the tongue and soft tissues from collapsing backward.
Examples include:
- SomnoDent®
- Thornton Adjustable Positioner (TAP)
- EMA (Elastic Mandibular Advancement)
- ProSomnus® EVO™
These devices are typically adjustable, allowing for incremental advancement of the jaw to find the optimal position that balances comfort with effectiveness.
2. Tongue Retaining Devices (TRDs)
Rather than moving the jaw, TRDs use suction to hold the tongue forward, preventing it from falling back and blocking the airway. These devices may be preferable for:
- People with dental issues that make MADs unsuitable
- Those with temporomandibular joint (TMJ) disorders
- Denture wearers (in some cases)
3. Combination Therapy Devices
Some newer devices combine features of oral appliances with other technologies:
- Devices that incorporate nasal dilators
- Appliances with built-in tongue muscle stimulation
- Hybrid PAP/oral appliance systems
A 2025 article in Sleep World Magazine highlighted Panthera Dental’s innovative CAD/CAM, 3D-printed oral appliances, which are currently being studied in a five-year multicenter trial to assess their long-term effectiveness.
Effectiveness of Oral Appliances: What the Research Shows
The effectiveness of oral appliances for sleep apnea has been the subject of extensive research. Here’s what the latest studies tell us:
Comparison with CPAP
A comprehensive umbrella review published in 2023 analyzed 27 systematic reviews comparing oral appliances to CPAP therapy. The findings showed:
- CPAP is more effective at reducing the Apnea-Hypopnea Index (AHI, a measure of sleep apnea severity) and improving minimum oxygen saturation levels.
- Despite CPAP’s greater efficacy, patient preference often favors oral appliances due to comfort and convenience.
- Adherence rates for oral appliances (approximately 77% after one year) often exceed those for CPAP (which can be as low as 50% in some studies).
Dr. Michael Chen, a dental sleep medicine specialist, explains: “The most effective treatment is the one the patient will actually use. A slightly less efficient therapy that’s used consistently often yields better real-world results than a more efficient one that sits unused in a drawer.”
Effectiveness by Sleep Apnea Severity
Research indicates that oral appliance effectiveness varies depending on the severity of sleep apnea:
- Mild OSA (AHI 5-15): Oral appliances can be highly effective, with success rates of 70-80%
- Moderate OSA (AHI 15-30): Effectiveness ranges from 60-75%
- Severe OSA (AHI >30): Success rates drop to 25-40%
However, even in severe cases where oral appliances don’t completely resolve the condition, they often significantly reduce its severity and associated symptoms.
Impact on Health Outcomes
Beyond reducing AHI scores, studies show oral appliances can improve various health metrics:
- Blood pressure: Modest but significant reductions in both systolic and diastolic readings
- Daytime sleepiness: Improved scores on standardized sleepiness scales
- Quality of life: Enhanced sleep quality and daily functioning
- Cardiovascular markers: Reductions in some inflammatory markers associated with heart disease
According to the 2025 Nature study, these improvements, while sometimes less dramatic than those seen with CPAP, represent meaningful clinical benefits for many patients.
Who Is a Good Candidate for Oral Appliance Therapy?
While oral appliances offer an excellent alternative to CPAP for many people, they aren’t the right solution for everyone. Based on current clinical guidelines, ideal candidates include:
Recommended Candidates
- Patients with primary snoring (without sleep apnea) who desire treatment
- Individuals with mild to moderate OSA who prefer an oral appliance to CPAP
- Patients with severe OSA who cannot tolerate CPAP or have failed CPAP treatment
- Those who travel frequently and need a portable treatment option
- People seeking a supplementary treatment to use with CPAP or other therapies
Factors That May Limit Success
Certain factors may reduce the effectiveness of oral appliances or make them unsuitable:
- Insufficient teeth to anchor the appliance (though some newer designs can work with partial dentures)
- Severe TMJ disorders that might be aggravated by jaw repositioning
- Central sleep apnea (a less common form caused by brain signaling issues rather than physical obstruction)
- Severe obesity (BMI >40), which may require more aggressive treatment approaches
- Significant nasal obstruction that prevents adequate nasal breathing
Dr. Jennifer Williams, a prosthodontist specializing in dental sleep medicine, notes: “A thorough evaluation by both a sleep physician and a qualified dental sleep medicine practitioner is essential to determine if an oral appliance is appropriate for your specific situation.”
The Treatment Journey: What to Expect with Oral Appliance Therapy
If you’re considering an oral appliance for sleep apnea, here’s what the process typically involves:
1. Diagnosis and Referral
The journey begins with proper diagnosis:
- Sleep testing (either in a lab or at home) to confirm OSA and assess its severity
- Referral from a sleep physician to a qualified dentist for oral appliance therapy
- Review of medical and dental history to identify any contraindications
2. Dental Evaluation
A comprehensive dental assessment ensures you’re a good candidate:
- Examination of teeth, gums, and jaw joint health
- Evaluation of airway anatomy
- Discussion of treatment options and expectations
- Taking impressions or digital scans of your teeth
3. Appliance Selection and Fabrication
Based on your specific needs, the dentist will:
- Select the most appropriate type of appliance
- Take precise measurements for custom fabrication
- Send specifications to a dental laboratory or use in-office technology to create your device
- Schedule a fitting appointment (typically 2-3 weeks after impressions)
4. Fitting and Adjustment
When your appliance is ready:
- The dentist will check the fit and make initial adjustments
- You’ll receive instructions on insertion, removal, and cleaning
- The dentist will determine a gradual advancement schedule to optimize effectiveness while minimizing side effects
5. Follow-Up and Titration
Ongoing care ensures optimal results:
- Regular adjustments (titration) to find the ideal jaw position
- Monitoring for side effects or comfort issues
- Dental check-ups to ensure oral health is maintained
- Follow-up sleep testing to confirm effectiveness
6. Long-Term Management
Successful therapy requires ongoing care:
- Annual evaluations of the appliance and your oral health
- Periodic reassessment of sleep apnea status
- Replacement of the appliance when worn (typically every 2-5 years)
- Coordination with your sleep physician for comprehensive care
Potential Side Effects and How to Manage Them
Like any treatment, oral appliances can cause side effects, though most are mild and temporary:
Common Side Effects
- Tooth or jaw discomfort: Usually resolves as you adjust to the appliance
- Management: Gradual adaptation schedule, over-the-counter pain relievers
- Excessive salivation or dry mouth: Typically improves within a few weeks
- Management: Staying hydrated, using xylitol gum or lozenges
- Temporary bite changes: Morning jaw exercises can help
- Management: Using a “morning repositioner” to realign the bite after removing the appliance
Less Common Concerns
- Permanent bite changes: Can occur with long-term use
- Management: Regular dental monitoring, appliance adjustments
- TMJ discomfort: May require appliance modification
- Management: Jaw exercises, appliance adjustments, temporary discontinuation if severe
- Gum irritation or tooth movement: Requires professional attention
- Management: Appliance adjustments, periodic dental evaluations
Dr. Robert Thompson, a dental sleep medicine practitioner, advises: “Most side effects can be effectively managed with proper follow-up care. The key is maintaining regular communication with your dental provider about any concerns.”
Insurance Coverage and Cost Considerations
The financial aspect of oral appliance therapy is an important consideration:
Insurance Coverage
Coverage varies widely:
- Medical insurance (not dental) typically covers oral appliances for diagnosed OSA
- Medicare covers oral appliances when certain criteria are met (using HCPCS code E0486)
- Documentation requirements include a sleep study, prescription from a sleep physician, and proof of CPAP intolerance in some cases
Out-of-Pocket Costs
If paying without insurance:
- Custom oral appliances typically range from $1,500-$3,000
- This includes the device, fitting, adjustments, and follow-up care
- Some dentists offer payment plans or financing options
Cost-Effectiveness
Research suggests oral appliances can be cost-effective in the long run:
- Fewer doctor visits for untreated sleep apnea complications
- Reduced risk of accidents due to daytime sleepiness
- Lower likelihood of developing expensive-to-treat comorbidities
Success Stories: Real Patients, Real Results
The impact of oral appliance therapy is best illustrated through patient experiences:
Michael’s Journey: From CPAP Frustration to Restful Sleep
Michael, a 52-year-old sales executive with moderate sleep apnea, struggled with CPAP for months. “I travel frequently for work, and lugging the CPAP machine through airports was a nightmare. Plus, I could never get comfortable with the mask,” he explains.
After switching to a mandibular advancement device, Michael found relief: “It took about two weeks to adjust completely, but now I sleep through the night, my energy has returned, and my wife says the snoring is gone. The best part is I can slip it in my pocket when traveling.”
Follow-up testing showed Michael’s AHI decreased from 22 to 4 events per hour—a significant improvement that moved him from moderate to mild sleep apnea.
Jennifer’s Experience: Finding the Right Solution
Jennifer, a 45-year-old teacher with mild sleep apnea, was initially hesitant about treatment. “I didn’t want anything invasive, and the thought of sleeping with a mask seemed claustrophobic,” she recalls.
Her dentist recommended a tongue-retaining device, which proved to be an excellent match: “It’s simple to use and comfortable enough that I forget it’s there. My morning headaches disappeared within the first week, and I’m no longer falling asleep during my planning period at school.”
Jennifer’s success highlights how finding the right device for each individual’s needs and preferences is crucial for treatment adherence and effectiveness.
The Future of Dental Sleep Medicine
The field of dental sleep medicine continues to evolve rapidly, with several exciting developments on the horizon:
Technological Advancements
- Digital design and manufacturing: CAD/CAM technology and 3D printing are creating more precise, comfortable appliances
- Remote monitoring capabilities: Sensors embedded in devices to track usage and effectiveness
- Combination therapies: Devices that integrate multiple treatment approaches
Research Directions
According to the 2025 Nature study, current research is focusing on:
- Identifying genetic and anatomical predictors of oral appliance success
- Developing more personalized treatment protocols
- Exploring the long-term health outcomes of oral appliance therapy
- Investigating new materials and designs for improved comfort and effectiveness
Expanding Role of Dentistry
The dental profession‘s involvement in sleep medicine continues to grow:
- Increased education in dental schools about sleep-disordered breathing
- More dentists pursuing specialized training in dental sleep medicine
- Greater collaboration between dentists and sleep physicians
- Expanded screening for sleep apnea in dental practices
Conclusion: Breathing Easier Through Dental Innovation
Sleep apnea represents a significant health challenge for millions of people worldwide, with consequences that extend far beyond disruptive snoring. While CPAP remains the gold standard treatment, oral appliance therapy offers an effective alternative that many patients find more comfortable and convenient.
The growing body of research supports oral appliances as a legitimate treatment option, particularly for those with mild to moderate OSA or those who cannot tolerate CPAP. With proper selection, fitting, and follow-up care, these dental devices can significantly improve both sleep quality and overall health.
If you’re struggling with sleep apnea or suspect you might have it, consider discussing oral appliance therapy with your healthcare providers. The solution to better breathing—and better health—might be as close as your dental office.
Remember, the most effective treatment is one that you’ll use consistently. For many, an oral appliance represents not just a treatment but a life-changing pathway to restful sleep and improved well-being.
Have you tried oral appliance therapy for sleep apnea? What has your experience been like? Share your thoughts in the comments below.