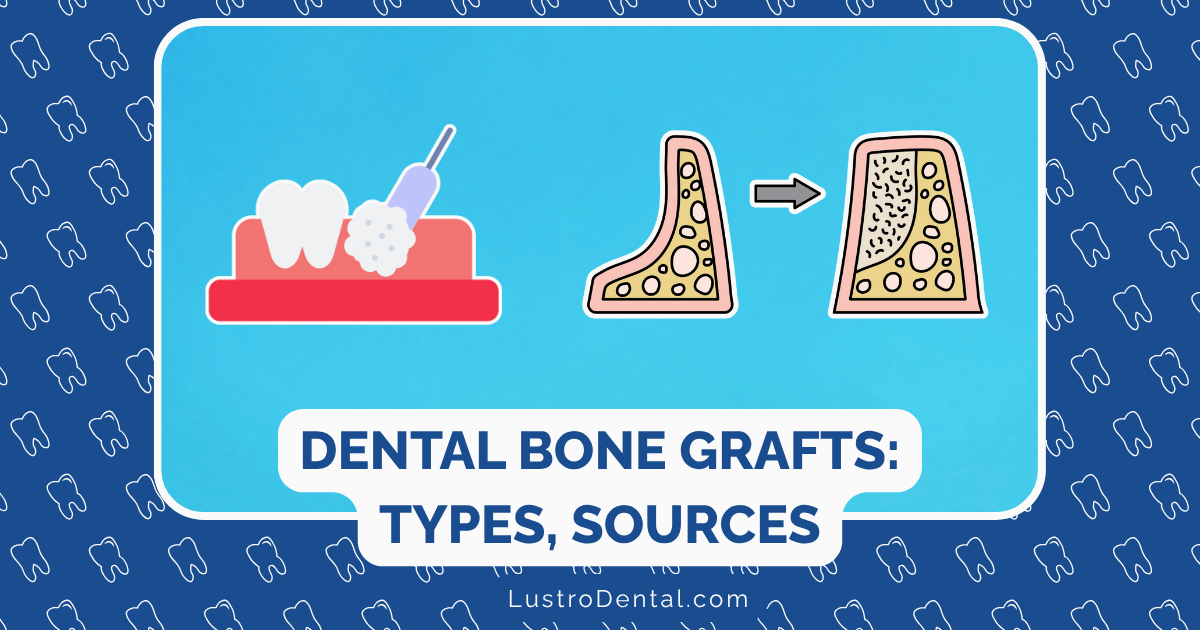
Types of Dental Bone Grafts: Sources, Procedures, and Applications
When Maria came to our practice, she was devastated. After losing a front tooth in an accident, she was told she wasn’t a candidate for a dental implant because she didn’t have enough bone. “Will I have to wear a removable partial denture forever?” she asked, clearly upset at the prospect.
Stories like Maria’s are common in dental offices across the country. Bone loss following tooth extraction, periodontal disease, or trauma can create significant challenges for tooth replacement. The good news? Modern bone grafting techniques have revolutionized our ability to rebuild lost bone and create a foundation for dental implants and other restorative procedures.
In this comprehensive guide, we’ll explore the fascinating world of dental bone grafts—the various types, where they come from, how they work, and which situations call for specific materials. Whether you’re considering a bone graft procedure or simply curious about this remarkable area of dentistry, this article will provide the knowledge you need.
Understanding Bone Biology: The Foundation of Successful Grafting
Before diving into the types of bone grafts, it’s essential to understand how bone naturally heals and regenerates. This knowledge helps explain why certain graft materials work better in specific situations.
The Remarkable Self-Healing Properties of Bone
Bone is one of the few tissues in the human body that can regenerate itself completely. When bone is damaged, a complex cascade of events occurs:
- Inflammatory phase: Blood clots form, bringing essential cells to the injury site
- Soft callus formation: Cartilage develops to bridge the gap
- Hard callus formation: The cartilage is gradually replaced with woven bone
- Remodeling phase: Woven bone is replaced by stronger lamellar bone
According to research published in the Journal of Dental Research, this natural process requires three key elements:
- Scaffolding: A framework for new bone cells to attach to
- Growth factors: Proteins that stimulate and direct bone formation
- Progenitor cells: Cells capable of developing into bone-forming cells
Dental bone grafts work by providing one or more of these elements to enhance the body’s natural healing process.
The Four Biological Mechanisms of Bone Grafts
Dental bone grafts support healing through four primary mechanisms:
1. Osteogenesis
Osteogenesis refers to the direct formation of new bone by living cells within the graft. Only grafts containing living bone cells (autografts) can provide true osteogenic properties.
2. Osteoconduction
Osteoconduction describes a graft’s ability to serve as a scaffold or framework that supports the growth of new bone. Most bone graft materials are osteoconductive, providing a matrix that allows bone-forming cells to attach and develop.
3. Osteoinduction
Osteoinduction involves the stimulation of undifferentiated cells to develop into bone-forming cells. This process is driven by growth factors like bone morphogenetic proteins (BMPs). Some graft materials naturally contain these growth factors, while others may have them added.
4. Osteointegration
Osteointegration refers to the direct structural and functional connection between living bone and the surface of the implant or graft material. This is crucial for long-term stability.
Dr. James Wilson of the American Academy of Periodontology explains: “Understanding these four mechanisms helps us select the optimal graft material for each patient’s unique situation. Different graft types excel in different mechanisms, which is why we often use specific materials for specific clinical scenarios.”
The Four Main Types of Dental Bone Grafts
Dental bone grafts are categorized based on their source. Each type has distinct advantages, limitations, and ideal applications.
1. Autografts: Your Body’s Own Bone
Source: Patient’s own body, typically from the chin, ramus (back part of lower jaw), hip, or tibia (shin bone)
Advantages:
- Contains living cells capable of forming new bone (osteogenic)
- No risk of disease transmission or rejection
- Provides the highest level of biocompatibility
- Contains natural growth factors that stimulate bone formation
Limitations:
- Requires a second surgical site, increasing discomfort and recovery time
- Limited availability of donor bone
- Potential for donor site complications
- Increased surgical time
Ideal Applications:
- Large defects requiring significant reconstruction
- Cases where maximum biological activity is crucial
- Younger patients with excellent healing capacity
- When other graft materials have failed
Dr. Sarah Chen of Mayo Clinic notes: “Autografts remain the gold standard against which all other graft materials are measured. The living cells they contain provide unmatched biological activity. However, the need for a second surgical site means we often reserve them for more complex cases.”
2. Allografts: Human Donor Bone
Source: Human cadavers, processed through tissue banks under strict FDA regulations
Advantages:
- No need for a second surgical site
- Available in various forms (particulate, putty, blocks)
- Contains some growth factors that stimulate bone formation
- Well-documented safety and efficacy
Limitations:
- No living cells (not osteogenic)
- Slight theoretical risk of disease transmission (though no documented cases with modern processing)
- Some patients have ethical or religious concerns
- Slower integration compared to autografts
Ideal Applications:
- Socket preservation after tooth extraction
- Horizontal ridge augmentation
- Sinus lift procedures
- Periodontal defects
Allografts undergo rigorous processing to ensure safety. According to the American Association of Tissue Banks, donor screening, testing, and tissue processing virtually eliminate disease transmission risk. These processes include:
- Comprehensive donor screening
- Serological testing for infectious diseases
- Tissue processing to remove cells and proteins
- Sterilization
- Strict tracking from donor to recipient
Two common types of allografts used in dentistry include:
- Freeze-dried bone allograft (FDBA): Maintains some of the natural growth factors
- Demineralized freeze-dried bone allograft (DFDBA): Processing exposes more bone morphogenetic proteins, potentially enhancing osteoinductive properties
3. Xenografts: Animal-Derived Bone
Source: Non-human species, typically bovine (cow), porcine (pig), or equine (horse)
Advantages:
- Unlimited supply
- No second surgical site
- Excellent space-maintenance properties
- Slow resorption rate provides long-term scaffold
- Natural bone structure similar to human bone
Limitations:
- No living cells (not osteogenic)
- Limited osteoinductive properties
- Some patients have ethical, religious, or personal concerns
- Potential for immune response (though rare with modern processing)
Ideal Applications:
- Sinus lift procedures
- Ridge preservation
- Cases requiring long-term structural stability
- Periodontal defects
Dr. Robert Johnson, researcher at the National Institutes of Health, explains: “Xenografts excel in situations where we need a stable scaffold that will maintain space over time. Their slow resorption rate can be advantageous in certain clinical scenarios, particularly in the maxillary sinus where we need the graft to resist pressure from the sinus.”
Modern xenografts undergo extensive processing to remove all organic components, leaving only the mineral structure. This processing eliminates the risk of disease transmission or rejection while preserving the natural architecture that supports bone growth.
4. Alloplasts: Synthetic Bone Substitutes
Source: Laboratory-created materials, typically made from calcium phosphates, bioactive glass, or polymers
Advantages:
- Unlimited availability
- No disease transmission risk
- No ethical concerns
- Consistent quality and composition
- Can be engineered for specific properties (porosity, resorption rate)
Limitations:
- No living cells (not osteogenic)
- Limited or no osteoinductive properties
- Variable clinical performance depending on the specific material
- Some types may migrate or break down unpredictably
Ideal Applications:
- Socket preservation
- Small to moderate defects
- Patients with concerns about human or animal-derived materials
- Combination with other graft materials
Several types of synthetic materials are commonly used in dental bone grafting:
Calcium Phosphate Ceramics
- Hydroxyapatite (HA): Closely resembles the mineral component of natural bone. Provides excellent structural support but resorbs very slowly.
- Beta-tricalcium phosphate (β-TCP): More readily resorbed than HA, allowing for gradual replacement by natural bone.
- Biphasic calcium phosphate (BCP): Combines HA and β-TCP to balance stability and resorbability.
Bioactive Glass
Made from silicon dioxide, sodium oxide, calcium oxide, and phosphorus pentoxide, bioactive glass forms a chemical bond with bone and stimulates osteoblast activity. Research published in the Journal of Biomedical Materials Research suggests bioactive glass may have antibacterial properties, making it valuable in infected sites.
Calcium Sulfate
One of the oldest synthetic bone graft materials, calcium sulfate (plaster of Paris) resorbs relatively quickly and is often used as a barrier membrane or in combination with other graft materials.
Polymer-Based Materials
Synthetic polymers like poly(lactic-co-glycolic acid) (PLGA) can be engineered to have specific degradation rates and mechanical properties. These materials are increasingly being used as carriers for growth factors and stem cells in advanced bone regeneration techniques.
Specialized Bone Graft Materials and Techniques
Beyond the four main categories, several specialized materials and techniques have emerged to enhance bone regeneration:
Growth Factors and Biologics
Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF)
Derived from the patient’s own blood, these concentrates contain growth factors that stimulate bone and soft tissue healing. According to a meta-analysis published in the International Journal of Implant Dentistry, combining PRP or PRF with bone grafts may enhance early healing and improve soft tissue outcomes.
Bone Morphogenetic Proteins (BMPs)
These powerful growth factors directly stimulate bone formation. The FDA has approved recombinant human BMP-2 (rhBMP-2) for specific dental applications, including sinus augmentation and localized alveolar ridge defects.
Dr. Emily Rodriguez of the American Academy of Implant Dentistry notes: “Growth factors represent the cutting edge of bone regeneration. They can dramatically enhance the performance of traditional graft materials, though their use requires careful case selection and technique.”
Combination Grafts
Many modern bone grafting procedures use combinations of different materials to harness the advantages of each. Common combinations include:
- Autograft + xenograft: Combines the biological activity of autograft with the structural stability of xenograft
- Allograft + growth factors: Enhances the osteoinductive potential of allograft
- Synthetic material + autogenous blood concentrates: Adds biological factors to synthetic scaffolds
Barrier Membranes
While not bone graft materials themselves, barrier membranes play a crucial role in guided bone regeneration (GBR) procedures. These membranes:
- Prevent soft tissue from growing into the bone graft site
- Create a protected space for bone regeneration
- Can be resorbable (collagen-based) or non-resorbable (expanded polytetrafluoroethylene)
Clinical Applications: Matching the Graft to the Situation
Different clinical scenarios call for different bone grafting approaches. Understanding these applications helps explain why your dentist might recommend a specific type of graft.
Socket Preservation
When a tooth is extracted, the surrounding bone begins to resorb immediately. Socket preservation grafts are placed at the time of extraction to maintain ridge dimensions and facilitate future implant placement.
Commonly Used Materials:
- Allografts (particulate or putty forms)
- Xenografts
- Synthetic materials
- Combinations with collagen plugs or PRF
A study in the Journal of Oral Implantology found that socket preservation reduces horizontal bone loss by an average of 2.6 mm compared to extraction alone.
Sinus Lift Procedures
The maxillary sinus often expands following tooth loss in the upper posterior region, leaving insufficient bone height for implant placement. Sinus lift procedures elevate the sinus membrane and place bone graft material to create adequate bone volume.
Commonly Used Materials:
- Xenografts (particularly bovine-derived)
- Combination of autograft and xenograft
- Allografts
- Synthetic materials with slow resorption rates
Dr. Wilson explains: “The sinus environment presents unique challenges. The graft must resist pressure from respiratory forces while providing a stable scaffold for new bone formation. Materials with slower resorption rates, like xenografts, often perform well in this environment.”
Horizontal Ridge Augmentation
When the alveolar ridge is too narrow for implant placement, horizontal augmentation techniques can increase ridge width.
Commonly Used Materials:
- Block autografts for larger defects
- Particulate allografts or xenografts contained by membranes
- Titanium-reinforced membranes with particulate grafts
- Growth factor-enhanced grafts for challenging cases
Vertical Ridge Augmentation
Increasing ridge height is generally considered the most challenging type of bone augmentation, with higher complication rates and technique sensitivity.
Commonly Used Materials:
- Block autografts from ramus or chin
- Distraction osteogenesis techniques
- Titanium-reinforced membranes with particulate autografts
- Growth factor-enhanced grafts
Periodontal Regeneration
Bone loss from periodontal disease creates unique defects around teeth that require specialized approaches to regenerate bone, cementum, and periodontal ligament.
Commonly Used Materials:
- DFDBA with growth factors
- Enamel matrix derivatives
- Bioactive glass
- PRF or PRP enhanced grafts
Making the Choice: Factors That Influence Graft Selection
Several factors influence the selection of bone graft materials for a specific patient:
Defect Size and Type
- Small defects may be successfully treated with allografts, xenografts, or synthetics
- Large defects often require autografts or combinations with growth factors
- Contained defects (surrounded by walls of bone) have better regenerative potential
- Non-contained defects may require membranes and structurally stable graft materials
Patient-Specific Factors
- Age: Younger patients generally have better regenerative capacity
- Smoking status: Smoking significantly impairs bone healing
- Medical conditions: Diabetes, osteoporosis, and other conditions affect graft success
- Medications: Bisphosphonates, immunosuppressants, and other medications may impact healing
- Personal preferences: Some patients have specific concerns about graft sources
Surgical Considerations
- Planned restoration: Implant placement requires different bone quality than pontic sites
- Available surgical expertise: Some techniques require specialized training
- Timing requirements: How quickly the area needs to be restored
- Cost considerations: Significant variation exists in the cost of different materials
Recovery and Success Rates: What to Expect
Understanding the healing process and expected outcomes helps patients set realistic expectations.
Typical Healing Timeline
- Initial healing (1-2 weeks): Soft tissue closure, initial inflammation subsides
- Early bone formation (1-3 months): Graft integration begins, early woven bone forms
- Maturation (3-9 months): Remodeling into lamellar bone, increasing density
- Final maturation (9+ months): Complete integration and remodeling
Dr. Rodriguez notes: “Patience is essential with bone grafting procedures. While we can accelerate healing to some extent with advanced techniques, the biological process of bone formation requires time. Rushing this process often leads to suboptimal results.”
Success Rates by Graft Type
Research published in the International Journal of Oral & Maxillofacial Implants reports the following success rates:
- Autografts: 95-100% success in healthy patients
- Allografts: 85-95% success
- Xenografts: 90-95% success
- Synthetic materials: 80-95% success (varies by material)
These rates vary based on the specific clinical situation, patient factors, and surgical technique.
Potential Complications
While bone grafting procedures are generally safe and predictable, potential complications include:
- Infection: More common in larger grafts and medically compromised patients
- Graft failure/resorption: Can occur due to poor blood supply, infection, or mechanical factors
- Membrane exposure: Can compromise guided bone regeneration results
- Prolonged swelling or pain: May indicate infection or inflammatory response
- Paresthesia: Temporary or permanent nerve disturbances (primarily with autografts)
Maria’s Story: A Successful Outcome
Remember Maria from the beginning of our article? After a comprehensive evaluation, we recommended a socket preservation procedure using a combination of allograft material and a collagen membrane. Six months later, the site had developed sufficient bone for implant placement.
“I never thought I’d be able to have a permanent tooth again,” Maria shared. “The bone grafting process was much easier than I expected, and now no one can tell I ever lost a tooth.”
The Future of Dental Bone Grafting
The field of bone regeneration continues to evolve rapidly. Emerging technologies promise even more predictable and less invasive approaches:
3D Printed Scaffolds
Custom-designed, 3D-printed scaffolds can precisely match the dimensions of bone defects. These scaffolds can be manufactured from resorbable materials and potentially seeded with the patient’s own stem cells.
Stem Cell Therapies
Research at institutions like the National Institute of Dental and Craniofacial Research is exploring the use of mesenchymal stem cells to enhance bone regeneration. Early clinical trials show promising results for challenging bone defects.
Gene Therapy Approaches
Delivering genes that encode for bone-stimulating proteins directly to the graft site may enhance regeneration while reducing the need for exogenous growth factors.
Dr. Chen explains: “The future of bone grafting lies in personalized approaches that harness the patient’s own biology. We’re moving toward solutions that stimulate natural healing processes rather than simply providing passive scaffolds.”
Conclusion: The Right Graft for the Right Situation
Dental bone grafting has transformed our ability to rebuild lost bone and restore both function and aesthetics. The wide variety of available materials allows for customized approaches to each patient’s unique situation.
As we’ve seen, no single graft material is ideal for all situations. The art and science of bone regeneration involve selecting the right material—or combination of materials—for each specific clinical scenario, patient preference, and biological need.
If you’re considering a procedure involving bone grafting, discuss these options with your dental specialist. Understanding the different types of grafts and their applications will help you participate more fully in decisions about your care and set realistic expectations for outcomes.
Have you experienced a dental bone grafting procedure? What type of graft was used, and what was your experience like? Share your story in the comments below to help others who might be facing similar procedures.