The Cavity Connection: How Dry Mouth Accelerates Tooth Decay
Have you ever wondered why dentists become so concerned when patients mention dry mouth symptoms? It’s not just about comfort—there’s a critical connection between xerostomia (the medical term for dry mouth) and an increased risk of tooth decay that every dental patient should understand.
As a dental health advocate who has worked with countless patients struggling with oral health challenges, I’ve seen firsthand how chronic dry mouth can transform a healthy mouth into one plagued by cavities in a matter of months. The science behind this connection is compelling, and understanding it could save your teeth.
The Silent Guardian: How Saliva Protects Your Teeth
Before we explore how dry mouth and accelerated tooth decay are connected, let’s appreciate the remarkable protective qualities of saliva that we often take for granted.
Saliva is far more than just water. This complex fluid contains minerals, enzymes, proteins, and antimicrobial compounds that work together to:
1. Neutralize Acids and Balance pH
Every time you eat, bacteria in your mouth feast on food particles (especially carbohydrates) and produce acids as a byproduct. These acids can drop your mouth’s pH to dangerous levels where enamel begins to demineralize—the first step toward cavity formation.
Saliva contains bicarbonate ions that neutralize these acids, typically returning your mouth to a safe pH level within 30-60 minutes after eating. Without adequate saliva, this acid neutralization process is severely compromised, leaving teeth exposed to acid attacks for extended periods.
2. Remineralize Enamel
Saliva is saturated with calcium and phosphate ions—the very building blocks of tooth enamel. These minerals continuously repair microscopic damage to your teeth through a process called remineralization. This natural repair system is your first line of defense against cavity formation.
According to the American Dental Association, when saliva flow is reduced, this remineralization process becomes inadequate, leaving teeth vulnerable to progressive decay.
3. Clear Food Debris and Bacteria
The physical washing action of saliva helps remove food particles and bacteria from tooth surfaces. This mechanical cleansing effect is so significant that areas with greater saliva exposure (like the front of lower teeth near salivary gland ducts) typically develop fewer cavities than areas with less salivary flow.
4. Provide Antimicrobial Protection
Saliva contains several antimicrobial components, including lysozyme, lactoferrin, and immunoglobulins, that help control the oral bacterial population. These natural antibacterial agents help keep cavity-causing bacteria in check.
The Perfect Storm: How Dry Mouth Creates Ideal Conditions for Decay
When salivary flow diminishes, several changes occur simultaneously that dramatically accelerate the tooth decay process:
1. Extended Acid Exposure
Without sufficient saliva to neutralize acids, the pH in your mouth remains in the danger zone (below 5.5) for much longer periods. Research shows that in a healthy mouth, pH typically returns to normal within an hour after eating. In xerostomia patients, this acid neutralization can take 3-4 times longer—or may never fully recover between meals.
This extended acid exposure means enamel is constantly under attack, with little opportunity for recovery. It’s like leaving your car in salt water all day instead of just driving through a puddle—the corrosive damage becomes inevitable and severe.
2. Disrupted Remineralization
The remineralization process requires both minerals and an appropriate pH environment. Dry mouth compromises both. Without the calcium and phosphate ions from saliva, and with a persistently acidic environment, teeth lose minerals faster than they can be replaced.
This mineral deficit eventually becomes visible as white spots on teeth—the first clinical sign of impending cavities. These areas represent demineralized enamel that has lost approximately 30% of its mineral content.
3. Bacterial Overgrowth
Studies show that patients with xerostomia typically have significantly higher levels of Streptococcus mutans and Lactobacilli—the primary bacteria associated with cavity formation. Without saliva’s antimicrobial properties, these harmful bacteria flourish unchecked.
Furthermore, the composition of the entire oral microbiome shifts in dry mouth conditions, favoring acid-producing and acid-tolerant species. This microbial imbalance creates a vicious cycle where more acid is produced, further lowering pH and promoting even more growth of cavity-causing bacteria.
4. Increased Plaque Accumulation
Saliva helps prevent plaque from adhering firmly to teeth. Without this protection, plaque accumulates more rapidly and adheres more tenaciously to tooth surfaces. This thick, sticky biofilm traps acids against the tooth surface and serves as a protective habitat for harmful bacteria.
Research published in the Journal of Dental Research has demonstrated that xerostomia patients can develop significantly more plaque within 24 hours than individuals with normal salivary flow, even with identical oral hygiene practices.
5. Altered Food Clearance
Without adequate saliva, food particles remain in contact with teeth for extended periods. This prolonged exposure to fermentable carbohydrates gives bacteria more time to produce acids. What might be a brief acid challenge in a healthy mouth becomes a prolonged attack in someone with dry mouth.
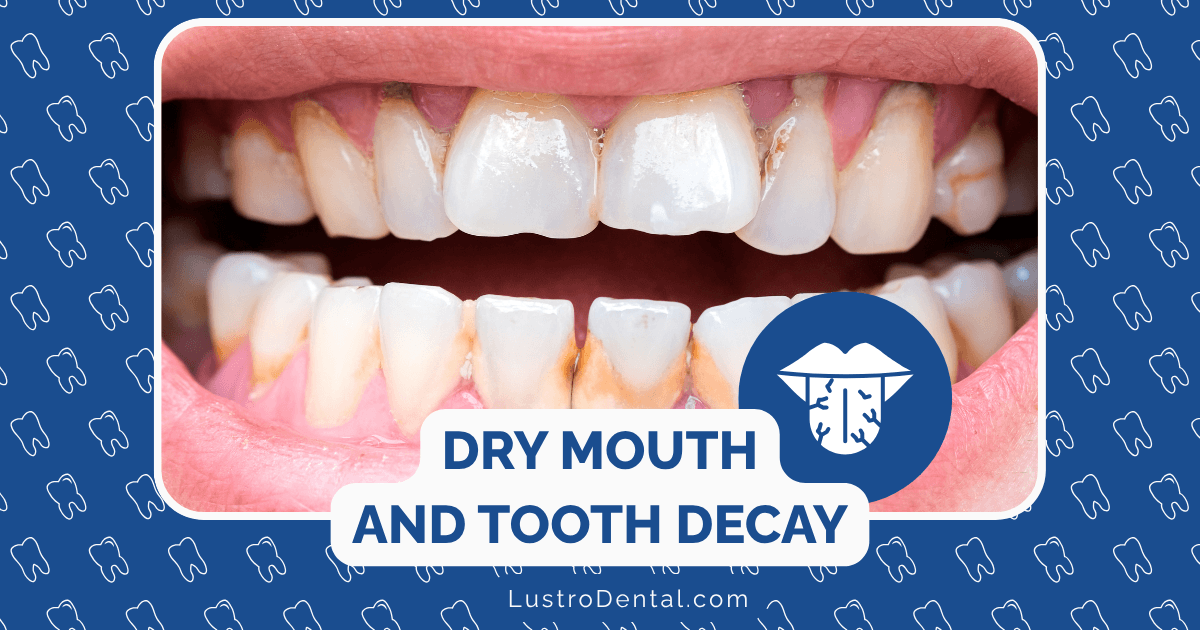
The Vulnerable Zones: Where Decay Strikes First
In patients with xerostomia, cavities often develop in unusual patterns that can help dentists identify the underlying dry mouth condition:
Root Surface Cavities
The first areas to show decay in xerostomia patients are often the exposed root surfaces near the gumline. These areas lack the protective enamel covering of the crown and are particularly vulnerable when not bathed in protective saliva.
Incisal and Cusp Tip Decay
In severe cases of dry mouth, decay can appear at the edges and tips of teeth—locations that rarely develop cavities in patients with normal salivary flow. This pattern is so distinctive that experienced dentists often recognize it immediately as a sign of xerostomia.
Cervical “Necklace” Cavities
A characteristic pattern of decay that encircles teeth at the gumline (resembling a necklace) is highly associated with dry mouth conditions. This pattern develops because these areas receive less mechanical cleansing from the tongue and cheeks and rely heavily on saliva for protection.
The Accelerated Timeline: How Quickly Damage Occurs
The progression from healthy teeth to severe decay can be alarmingly rapid in patients with xerostomia:
- 1-3 months: Initial white spot lesions (demineralization)
- 3-6 months: Early cavitation (breakdown of enamel surface)
- 6-12 months: Moderate to deep cavities requiring extensive restoration
- 12+ months: Potential tooth loss if left untreated
This accelerated timeline stands in stark contrast to the much slower progression typically seen in patients with normal salivary flow, where the development of a cavity might take years rather than months.
Breaking the Cycle: Strategies to Protect Your Teeth
If you’re dealing with dry mouth, implementing a comprehensive protection strategy is essential to prevent this accelerated decay process:
1. Enhanced Fluoride Protection
Standard fluoride exposure is insufficient for most xerostomia patients. Consider:
- Prescription-strength fluoride toothpaste (5000 ppm fluoride) used twice daily
- Daily fluoride rinses (0.05% sodium fluoride)
- Professional fluoride varnish applications every 3-4 months
- Custom fluoride trays for home application of 1.1% neutral sodium fluoride gel
Research shows that diligent use of prescription fluoride products can reduce cavity formation by up to 70-80% in dry mouth patients.
2. Modified Oral Hygiene Practices
Mechanical plaque removal becomes even more crucial when saliva is limited:
- Brush at least twice daily with a soft-bristled electric toothbrush
- Use interdental cleaners (floss, interdental brushes) daily
- Consider adding a water flosser for enhanced cleaning
- Schedule professional cleanings every 3-4 months rather than the standard 6 months
3. Xylitol: The Protective Sweetener
Xylitol is a natural sugar substitute that offers significant benefits for dry mouth patients:
- Inhibits growth of Streptococcus mutans
- Creates an unfavorable environment for acid-producing bacteria
- Stimulates saliva flow in patients with residual salivary function
- Helps neutralize plaque acids
Aim for 6-10 grams of xylitol daily, divided into at least 3 exposures, through sugar-free gum, mints, or lozenges specifically formulated with xylitol.
4. Saliva Substitutes and Stimulants
While artificial saliva products can’t fully replicate the protective properties of natural saliva, they can provide significant relief and some protection:
- Saliva substitutes containing carboxymethylcellulose or hydroxyethylcellulose
- Oral moisturizing gels applied before bedtime
- Prescription sialagogues (medications that stimulate saliva production) such as pilocarpine or cevimeline for patients with functioning salivary glands
5. Dietary Modifications
What you eat and drink can dramatically impact your cavity risk when dealing with dry mouth:
- Limit fermentable carbohydrates, especially between meals
- Avoid acidic foods and beverages that can further lower oral pH
- Choose tooth-friendly snacks like cheese, nuts, or vegetables
- Rinse with water after eating when brushing isn’t possible
- Maintain adequate hydration by sipping water throughout the day
When to Seek Professional Help
If you’re experiencing persistent dry mouth, professional evaluation is essential. Consult with your dentist and physician if you notice:
- Persistent feeling of oral dryness
- Difficulty speaking, chewing, or swallowing
- Frequent thirst, especially at night
- Burning sensation in the mouth
- Cracked lips or corners of the mouth
- Increased tooth sensitivity
- New or rapidly progressing cavities
Early intervention can prevent the devastating oral health consequences of untreated xerostomia.
The Future of Xerostomia Management
Research into more effective treatments for dry mouth continues to advance. Promising developments include:
- Stem cell therapy to regenerate damaged salivary glands
- Gene therapy approaches to restore salivary gland function
- Advanced polymeric systems that more closely mimic natural saliva
- Electrostimulation devices to enhance natural saliva production
The MARSH clinical trial is currently evaluating stem cell regenerative therapy for patients with xerostomia after radiation therapy, potentially offering hope for those with severe salivary gland damage.
Conclusion: Breaking the Connection
The link between dry mouth and accelerated tooth decay is undeniable, but with knowledge and proactive management, you can break this connection. Understanding the mechanisms behind this relationship empowers you to take specific, targeted actions to protect your oral health.
If you’re dealing with xerostomia, remember that you’re not fighting this battle alone. Work closely with your dental professional to develop a personalized protection strategy that addresses your specific needs and risk factors. With vigilance and appropriate interventions, you can maintain your oral health despite the challenges of dry mouth.
Have you experienced dry mouth and its effects on your dental health? Share your experiences and strategies in the comments below.