Gum Disease Explained: Your Questions Answered with Compassion and Clarity
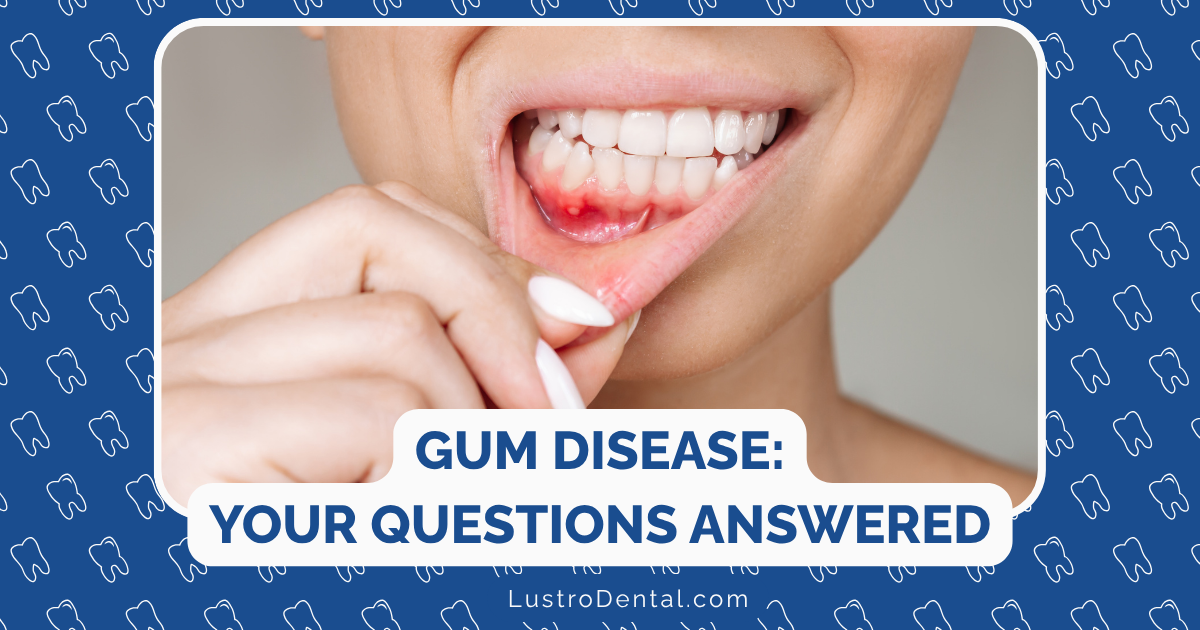
When you notice your gums bleeding while brushing or feel tenderness along your gumline, it’s natural to feel concerned. Gum disease affects millions of people worldwide, yet it remains widely misunderstood and often goes untreated until significant damage has occurred.
In this comprehensive guide, we’ll explore gum disease with both scientific accuracy and compassionate understanding. Whether you’re experiencing symptoms yourself, supporting a loved one, or simply seeking to prevent future problems, this article aims to provide clear answers to your most pressing questions about gum health.
Understanding Gum Disease: The Basics
Gum disease, medically known as periodontal disease, is an inflammatory condition affecting the tissues surrounding and supporting the teeth. Despite its prevalence—affecting nearly half of adults over 30 in the United States according to the Centers for Disease Control and Prevention—many people don’t fully understand what it is or how it develops.
What Exactly Is Gum Disease?
At its core, gum disease is an infection of the tissues that hold your teeth in place. These tissues include:
- Gingiva (gums): The visible pink tissue surrounding your teeth
- Periodontal ligament: Connective tissue fibers that attach the tooth to the bone
- Cementum: The layer of connective tissue that covers the tooth’s root
- Alveolar bone: The bone that surrounds and supports your teeth
When bacteria in plaque (the sticky film that forms on teeth) are not removed through regular brushing and flossing, they can cause inflammation of these tissues, beginning with the gums.
The Two Main Stages
Gum disease typically develops in two distinct stages:
1. Gingivitis
This is the earliest and mildest form of gum disease. During this stage:
- Bacteria in plaque irritate the gums, causing inflammation
- Gums become red, swollen, and may bleed easily during brushing or flossing
- There is usually little to no discomfort
- No irreversible damage to bone or connective tissue has occurred
- The condition is fully reversible with proper oral hygiene and professional care
2. Periodontitis
If gingivitis is left untreated, it can progress to periodontitis, a more serious condition where:
- Inflammation extends beyond the gums to the periodontal ligament and alveolar bone
- The gums pull away from the teeth, forming pockets that become infected
- These pockets deepen as the disease progresses
- Bone and connective tissue begin to break down
- Teeth may become loose and eventually require extraction
- The damage at this stage is largely irreversible, though it can be managed
Understanding this progression highlights why early intervention is so crucial. Catching and addressing gum disease at the gingivitis stage can prevent permanent damage to your oral structures.
Recognizing the Warning Signs
One of the challenges with gum disease is that it often develops painlessly, allowing it to progress unnoticed. Being aware of the warning signs can help you seek treatment before significant damage occurs.
Early Signs of Gingivitis
- Bleeding gums during brushing or flossing: Perhaps the most common and earliest sign
- Red or purple-tinged gums: Healthy gums should be pink
- Swollen or puffy gum tissue: Gums may appear enlarged
- Tenderness when touched: Gums may be sensitive to pressure
- Persistent bad breath: Caused by bacteria in the mouth
- Slight recession of the gumline: Teeth may appear longer than normal
Advanced Signs of Periodontitis
- Receding gums: Significant pulling back of gum tissue, exposing more of the tooth
- New spaces developing between teeth: Teeth may appear to be spreading apart
- Pus between teeth and gums: Indicates active infection
- Painful chewing: Discomfort when biting or eating
- Loose teeth: Movement or shifting of teeth in their sockets
- Changes in how teeth fit together: Alterations in your bite
- Pain or sensitivity: Particularly to hot or cold temperatures
Silent Symptoms
It’s important to note that some people with gum disease—even in advanced stages—may experience few or no noticeable symptoms. This is why regular dental check-ups are essential; your dental professional can detect signs of gum disease that you might miss.
According to research published in the Journal of Dental Research, up to 27% of people with moderate to severe periodontitis report no symptoms at all, highlighting the importance of professional evaluation.
The Progression: From Gingivitis to Periodontitis
Understanding how gum disease progresses can help you recognize the importance of early intervention and consistent care.
The Timeline of Progression
Stage 1: Initial Gingivitis (Days to Weeks)
When plaque accumulates along the gumline, bacteria in the plaque release toxins that irritate gum tissue. Within days, this can lead to:
- Microscopic inflammation
- Increased blood flow to the area
- Slight swelling and redness
- Potential bleeding during brushing
At this stage, the condition is easily reversible with improved oral hygiene and professional cleaning.
Stage 2: Established Gingivitis (Weeks to Months)
If the initial gingivitis isn’t addressed, it becomes more established:
- Visible redness and swelling increase
- Bleeding becomes more consistent
- Mild discomfort may develop
- Bad breath becomes more noticeable
Even at this stage, the condition remains reversible, though it may require more intensive professional cleaning.
Stage 3: Early Periodontitis (Months to Years)
The transition from gingivitis to early periodontitis marks a critical threshold:
- Inflammation begins to affect the periodontal ligament and alveolar bone
- Shallow pockets (3-4mm deep) form between teeth and gums
- Early bone loss may begin (detectable on X-rays)
- Gum recession becomes more noticeable
At this stage, some permanent damage has occurred, but progression can be halted with appropriate treatment.
Stage 4: Moderate Periodontitis (Years)
As the disease continues:
- Pockets deepen (4-6mm)
- Bone loss becomes more significant
- Teeth may begin to feel slightly loose
- Gum recession is more pronounced
- Root surfaces may become exposed, leading to sensitivity
Stage 5: Advanced Periodontitis (Years to Decades)
In the final stage:
- Deep pockets (>6mm)
- Significant bone loss (50% or more around some teeth)
- Teeth become loose and may shift position
- Chewing becomes painful
- Teeth may eventually be lost
Factors Affecting Progression
Not everyone progresses through these stages at the same rate. Several factors can accelerate or slow the development of periodontitis:
- Oral hygiene habits: Consistent brushing and flossing significantly slow progression
- Smoking: Accelerates disease progression and reduces treatment effectiveness
- Diabetes: Particularly when poorly controlled, can speed progression
- Genetics: Some people are more susceptible due to genetic factors
- Immune system function: Compromised immunity can accelerate progression
- Stress levels: Chronic stress can impair immune response to infection
- Medications: Some drugs reduce saliva flow, which normally helps protect against bacteria
Understanding this progression underscores why early intervention is so crucial—the earlier treatment begins, the less permanent damage occurs.
The Hidden Connection: Gum Disease and Overall Health
One of the most significant developments in our understanding of gum disease is the recognition that it’s not just an oral health issue—it has implications for your entire body. This bidirectional relationship means that gum disease can affect systemic health, and systemic conditions can influence gum disease.
How Gum Disease Affects Your Body
Research has established links between periodontitis and several serious health conditions:
Cardiovascular Disease
Multiple studies, including research published in the American Journal of Cardiology, have found associations between gum disease and heart disease:
- Bacteria from periodontal infections can enter the bloodstream
- These bacteria may contribute to arterial plaque formation
- The inflammatory response to gum disease may increase inflammation throughout the body
- People with gum disease have a 1.5 to 2 times higher risk of heart disease
Diabetes
The relationship between diabetes and periodontitis is particularly strong and bidirectional:
- People with diabetes are more susceptible to infections, including gum disease
- Periodontal inflammation can make blood sugar control more difficult
- Treating gum disease has been shown to improve glycemic control in some diabetic patients
- The American Diabetes Association recognizes this connection in their clinical guidelines
Respiratory Conditions
Research suggests connections between gum disease and respiratory issues:
- Bacteria from the mouth can be aspirated into the lungs
- This may contribute to pneumonia and other respiratory infections
- People with chronic respiratory conditions may experience more frequent exacerbations if they have untreated gum disease
Pregnancy Complications
Some studies indicate potential links between periodontitis and:
- Preterm birth
- Low birth weight
- Preeclampsia
While more research is needed, maintaining good oral health during pregnancy is considered an important preventive measure.
Other Potential Connections
Emerging research is investigating links between periodontitis and:
- Rheumatoid arthritis
- Certain cancers
- Alzheimer’s disease
- Kidney disease
How Your Health Affects Your Gums
Just as gum disease can impact overall health, certain health conditions and lifestyle factors can increase the risk and severity of periodontal problems:
- Diabetes: High blood sugar impairs immune function and healing
- Osteoporosis: May accelerate alveolar bone loss
- Medications: Many drugs cause dry mouth, reducing the protective effects of saliva
- Stress: Impairs immune response and may lead to teeth grinding
- Hormonal changes: Pregnancy, menopause, and other hormonal shifts can increase gum sensitivity
- Nutritional deficiencies: Particularly vitamin C, which is essential for gum health
This two-way relationship highlights why treating gum disease isn’t just about saving your teeth—it’s about protecting your overall health.
Conventional Treatment Approaches
Treating gum disease typically involves a combination of professional dental care and improved home oral hygiene. The specific approach depends on the stage and severity of the condition.
Treatment for Gingivitis
Since gingivitis is reversible, treatment focuses on removing plaque and irritants:
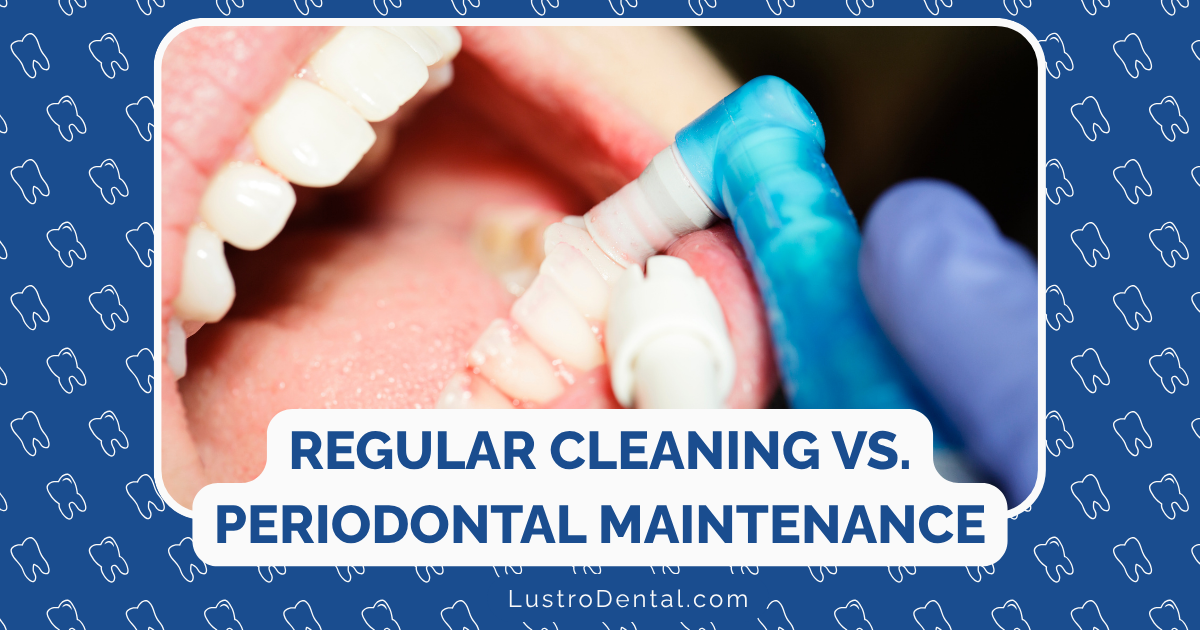
Professional Treatment
- Professional dental cleaning (prophylaxis): Removes plaque and tartar above and slightly below the gumline
- Oral hygiene instruction: Personalized guidance on effective brushing and flossing techniques
- Identification of risk factors: Addressing contributing issues like misaligned teeth or problematic dental restorations
Home Care
- Improved brushing: Twice daily with proper technique
- Daily flossing: To remove plaque between teeth
- Antimicrobial mouthwash: To reduce bacteria between cleanings
With consistent care, gingivitis typically resolves within 10-14 days, though maintaining these habits is essential to prevent recurrence.
Treatment for Periodontitis
Once the disease has progressed to periodontitis, more intensive interventions are necessary:
Non-Surgical Treatments
- Scaling and root planing: A deep-cleaning procedure performed under local anesthesia that removes plaque and tartar from below the gumline and smooths root surfaces to promote healing and reattachment of gum tissue
- Antibiotic therapy: May include:
- Topical antibiotics applied directly to infected pockets
- Antibiotic mouth rinses
- Oral antibiotics for more widespread infection
- More frequent professional cleanings: Typically every 3-4 months rather than the standard 6 months
Surgical Treatments for Advanced Cases
- Flap surgery (pocket reduction): Lifting back gum tissue to remove tartar deposits and reduce pocket depth
- Bone grafts: Replacing bone destroyed by periodontitis to provide support for teeth
- Soft tissue grafts: Reinforcing thin gums or filling in areas where gums have receded
- Guided tissue regeneration: Using special materials to encourage natural regrowth of bone and tissue
- Bone surgery: Smoothing shallow craters in bone to eliminate areas where bacteria can hide
Maintenance Therapy
After active treatment, ongoing maintenance is crucial:
- Regular professional cleanings (every 3-4 months)
- Periodic reassessment of pocket depths
- Consistent home care
- Management of risk factors
It’s important to understand that while damage from periodontitis isn’t fully reversible, the disease progression can be halted, and with appropriate treatment, many patients maintain their teeth for a lifetime.
The Role of the Oral Microbiome in Gum Health
Recent scientific advances have transformed our understanding of gum disease by highlighting the crucial role of the oral microbiome—the community of microorganisms living in your mouth. This new perspective offers promising approaches for prevention and treatment.
Understanding the Oral Microbiome
Your mouth naturally contains hundreds of species of bacteria, fungi, viruses, and other microorganisms living in a complex ecosystem. In a healthy mouth, these microbes exist in a balanced relationship with each other and with your body.
The Balance of Health and Disease
- Healthy microbiome: Dominated by beneficial or neutral species that help protect against disease
- Dysbiosis: An imbalance where harmful species become more prevalent, increasing disease risk
Research published in the Journal of Dental Research shows that people with periodontal disease have significantly different oral microbiome compositions compared to those with healthy gums.
How Dysbiosis Leads to Gum Disease
The development of gum disease isn’t simply about the presence of “bad bacteria” but rather about shifts in the microbial community:
- Initial colonization: Certain bacteria attach to teeth and form biofilms (plaque)
- Community shifts: As plaque matures, the bacterial composition changes
- Pathogen emergence: Species associated with gum disease become more dominant
- Immune response: Your body’s inflammatory response to these bacteria damages gum tissue
- Disease progression: The environment becomes increasingly favorable for disease-associated bacteria
Key bacteria associated with periodontal disease include Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia—often called the “red complex” due to their strong association with severe disease.
Traditional Approaches vs. Microbiome Perspective
Traditional treatments for gum disease often take a “scorched earth” approach, attempting to eliminate bacteria broadly. However, this can disrupt beneficial bacteria along with harmful ones.
A microbiome-focused approach instead aims to:
- Restore balance rather than eliminate all bacteria
- Support beneficial species that naturally inhibit pathogens
- Create an environment that favors health-associated microbes
Oral Probiotics: Supporting Microbiome Balance
One of the most promising developments in gum disease prevention and management is the use of oral probiotics—beneficial bacteria specifically selected to support oral health.
How Oral Probiotics Work
Unlike traditional treatments that indiscriminately kill bacteria, oral probiotics work by:
- Competing with harmful bacteria for space and resources
- Producing antimicrobial compounds that target pathogens
- Modulating the immune response to reduce inflammation
- Creating an environment less favorable for disease-associated bacteria
ProDentim: A Targeted Approach
ProDentim represents an innovative approach to supporting gum health through microbiome balance. Each tablet contains 3.5 billion CFUs (colony-forming units) of beneficial bacteria specifically selected for their role in oral health:
- Lactobacillus paracasei: Helps inhibit the growth of periodontal pathogens and supports immune function in the oral cavity
- Lactobacillus reuteri: Produces antimicrobial compounds that target harmful bacteria while supporting gum tissue health
- Bifidobacterium lactis BL-04: Helps maintain microbial balance and supports immune function
The formula also includes inulin (a prebiotic that selectively feeds beneficial bacteria) and other supporting ingredients that promote oral health.
Benefits for Gum Health
Many users of ProDentim report significant improvements in their gum health, including:
- Reduced gum bleeding during brushing and flossing
- Decreased gum tenderness and inflammation
- Fresher breath throughout the day
- Less visible redness in the gum tissue
While oral probiotics like ProDentim should complement rather than replace traditional oral hygiene and professional care, they offer a promising addition to comprehensive gum health strategies.
Innovative Approaches to Gum Disease Prevention
Beyond conventional treatments and oral probiotics, several innovative approaches are expanding our options for preventing and managing gum disease.
Precision Periodontal Medicine
This emerging field takes a personalized approach to gum disease, recognizing that the condition varies significantly between individuals:
- Genetic testing: Identifying genetic factors that increase susceptibility
- Microbiome analysis: Determining the specific bacterial profile in an individual’s mouth
- Biomarker assessment: Measuring inflammatory markers in saliva or gingival fluid
- Tailored interventions: Creating personalized prevention and treatment plans based on individual risk factors
Photodynamic Therapy
This non-invasive approach combines light activation with photosensitizing agents:
- A photosensitizing solution is applied to the gums
- When activated by a specific wavelength of light, it produces oxygen species that kill bacteria
- The treatment is highly targeted and doesn’t promote antibiotic resistance
- Research shows it can be effective as an adjunct to conventional treatment
Host Modulation Therapy
Rather than targeting bacteria directly, this approach aims to modify the host’s (your body’s) response to bacterial presence:
- Reduces excessive inflammatory responses that damage tissue
- May include low-dose doxycycline (below antimicrobial levels)
- Shows promise for patients with risk factors like diabetes or smoking
Nutritional Approaches
Emerging research highlights the role of nutrition in gum health:
- Omega-3 fatty acids: May help reduce gum inflammation
- Antioxidants: Vitamins C and E support tissue healing and immune function
- Vitamin D: Plays a role in immune regulation and bone health
- Coenzyme Q10: May support gum tissue healing
Comprehensive Approach: Combining Methods
The most effective approach to gum disease prevention and management typically combines multiple strategies:
- Foundation: Consistent brushing, flossing, and professional cleanings
- Microbiome support: Using products like ProDentim to maintain bacterial balance
- Risk factor management: Addressing smoking, stress, and systemic conditions
- Nutritional support: Ensuring adequate intake of key nutrients
- Regular monitoring: Professional assessment to catch changes early
This multi-faceted approach addresses the complex nature of periodontal disease and offers the best chance for long-term gum health.
Living with Gum Disease: Practical Daily Management
For those diagnosed with gum disease or at high risk, daily management becomes crucial for preventing progression and maintaining oral health.
Creating an Effective Home Care Routine
Morning Routine
- Thorough brushing: Using a soft-bristled toothbrush and fluoride toothpaste
- Brush for a full two minutes
- Use gentle circular motions at a 45-degree angle to the gumline
- Pay special attention to the gum margin where plaque accumulates
- Interdental cleaning: Removing plaque between teeth
- Floss, interdental brushes, or water flossers depending on your specific needs
- Follow your dental professional’s recommendation for the best tools for your situation
- Oral probiotic: Taking ProDentim after brushing
- Allows beneficial bacteria to establish themselves throughout the day
- Helps maintain microbiome balance between cleanings
Throughout the Day
- Hydration: Drinking plenty of water
- Helps maintain saliva flow, which has natural antimicrobial properties
- Rinses away food particles and bacteria
- Rinsing after meals: When brushing isn’t possible
- Plain water rinsing can help remove food debris
- Alcohol-free antimicrobial rinses for higher-risk individuals
Evening Routine
- Thorough brushing and interdental cleaning: Even more important before sleep
- Saliva flow naturally decreases during sleep, reducing its protective effect
- Removing plaque before bed prevents bacteria from thriving overnight
- Additional tools as recommended: May include:
- Prescription mouth rinses
- Gum massage tools
- Rubber-tip stimulators for the gumline
Lifestyle Factors for Gum Health
Nutrition
- Anti-inflammatory foods: Fatty fish, leafy greens, nuts, and berries
- Vitamin C-rich foods: Citrus fruits, bell peppers, and strawberries support collagen production
- Crunchy vegetables: Carrots, celery, and apples provide gentle cleaning action
- Limited sugars and refined carbohydrates: Reduce fuel for harmful bacteria
Stress Management
Since stress can impair immune function and worsen inflammation:
- Regular exercise
- Adequate sleep
- Mindfulness practices
- Stress reduction techniques
Avoiding Harmful Habits
- Quit tobacco: Smoking is one of the strongest risk factors for gum disease
- Limit alcohol: Excessive alcohol can dry the mouth and impair immune function
- Avoid recreational drugs: Many increase dry mouth and can worsen gum problems
Tracking Your Progress
Maintaining a simple tracking system can help you stay consistent and monitor improvements:
- Calendar marking for daily oral care
- Notes about symptoms like bleeding or tenderness
- Records of professional treatment recommendations
- Before and after photos (if comfortable) to visualize improvement
With consistent care, many people with early to moderate gum disease can achieve significant improvements within 2-3 months, though maintenance remains essential for life.
When to Seek Professional Help
While home care is essential, professional dental care plays a crucial role in preventing and treating gum disease. Understanding when to seek help can prevent minor issues from becoming serious problems.
Warning Signs That Require Prompt Attention
Contact your dental professional promptly if you experience:
- Persistent bleeding gums: Especially if it continues after improving oral hygiene
- Receding gums: Teeth that appear longer or visible root surfaces
- Loose teeth: Any mobility or shifting of teeth
- Persistent bad breath: Despite good oral hygiene
- Pus between teeth and gums: Indicates active infection
- Pain or sensitivity: Discomfort when chewing or with temperature changes
- Changes in bite: Teeth fitting together differently than before
What to Expect at a Periodontal Evaluation
A comprehensive periodontal assessment typically includes:
- Medical and dental history review: Including risk factors and medications
- Visual examination: Checking for redness, swelling, and other visible signs
- Probing: Measuring the depth of pockets between teeth and gums
- 1-3mm is generally considered healthy
- 4mm indicates early periodontitis
- 5mm or greater suggests moderate to advanced disease
- Bleeding assessment: Noting areas that bleed during probing
- Mobility testing: Checking for loose teeth
- Radiographs (X-rays): Evaluating bone levels around teeth
- Treatment planning: Developing a personalized approach based on findings
Finding the Right Dental Professional
For gum disease treatment, you might work with:
- General dentist: For mild to moderate cases
- Periodontist: A specialist in gum diseases, especially for advanced cases
- Dental hygienist: Works with dentists to provide cleanings and education
When selecting a provider, look for:
- Experience treating gum disease
- Willingness to explain findings and treatment options
- Comfort with questions and concerns
- Compassionate, non-judgmental approach
Remember that seeking help isn’t a sign of failure—it’s a proactive step toward better health. Many dental professionals now take a supportive, educational approach rather than a scolding one, recognizing that fear of judgment often prevents people from seeking needed care.
Moving Forward: Creating Your Gum Health Plan
Armed with knowledge about gum disease, you’re now ready to take proactive steps toward better gum health. Here’s a framework for creating your personalized plan:
Step 1: Assess Your Current Status
Start by honestly evaluating:
- Existing symptoms (bleeding, tenderness, recession)
- Current oral hygiene habits
- Risk factors you may have (smoking, diabetes, family history)
- When you last had a professional dental evaluation
Step 2: Schedule a Professional Assessment
If you haven’t had a dental check-up in the past six months, or if you’re experiencing symptoms:
- Schedule an appointment for a comprehensive periodontal evaluation
- Be open about any concerns or symptoms
- Ask questions about your specific condition and needs
Step 3: Develop Your Daily Care Routine
Based on professional recommendations and your specific situation:
- Select appropriate tools (toothbrush type, interdental cleaning devices)
- Establish a consistent morning and evening routine
- Consider incorporating ProDentim to support your oral microbiome
- Set reminders or use tracking methods to maintain consistency
Step 4: Address Modifiable Risk Factors
Identify factors you can change to improve your outcomes:
- Work toward quitting smoking if applicable
- Improve management of conditions like diabetes
- Address dry mouth if present
- Make dietary adjustments to support gum health
Step 5: Create a Monitoring System
Track your progress to stay motivated and catch any changes early:
- Note improvements in symptoms like bleeding or tenderness
- Keep a record of professional treatment recommendations
- Schedule and maintain regular professional maintenance visits
- Periodically reassess your home care effectiveness
Step 6: Build a Support System
Managing gum health is easier with support:
- Share your goals with family members
- Consider involving your household in improved oral hygiene
- Join online communities focused on oral health
- Maintain open communication with your dental professionals
Remember: Progress, Not Perfection
It’s important to approach gum health with self-compassion:
- Celebrate improvements rather than focusing on setbacks
- Recognize that consistent effort over time brings results
- Understand that occasional lapses don’t erase your progress
- View gum health as an ongoing journey rather than a destination
With the right knowledge, tools, and support—including innovative approaches like ProDentim—you can take control of your gum health and protect both your smile and your overall wellbeing for years to come.
Have you struggled with gum disease or found effective strategies for maintaining gum health? Share your experience in the comments below to help others on their journey.