Advances in Synthetic Bone Materials: Alternatives to Traditional Grafting
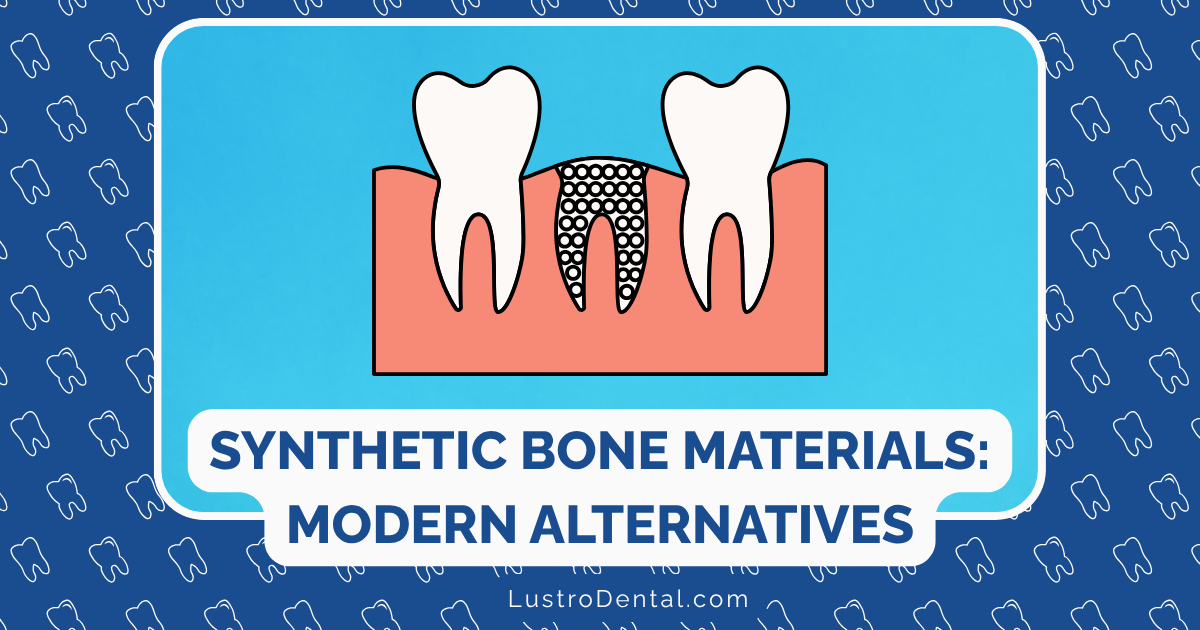
When Sarah visited our practice needing a dental implant, she was dismayed to learn she had insufficient bone for the procedure. “The oral surgeon I saw previously told me I’d need a bone graft from my hip,” she explained. “I’m not thrilled about having a second surgical site and the recovery that would involve. Are there any alternatives?”
Sarah’s question reflects a common concern among patients needing bone augmentation procedures. Fortunately, the field of dental biomaterials has experienced remarkable advancements in recent years, particularly in the development of synthetic bone substitutes that eliminate the need for harvesting bone from a second site.
In this comprehensive guide, we’ll explore the exciting world of synthetic bone materials—how they’ve evolved, what options are currently available, their advantages and limitations, and what the future holds for this rapidly advancing field.
The Evolution of Bone Grafting: From Autografts to Synthetic Alternatives
To appreciate how far we’ve come, it helps to understand the historical context of bone grafting materials.
Traditional Bone Grafting Approaches
For decades, autografts—bone harvested from the patient’s own body—were considered the gold standard for bone augmentation. While effective, this approach has significant drawbacks:
- Requires a second surgical site, increasing pain and recovery time
- Limited availability of donor bone
- Potential for complications at the donor site
- Extended surgical time and associated costs
According to Dr. James Wilson, a researcher at the National Institute of Dental and Craniofacial Research, “The search for alternatives to autografts has been driven by the desire to eliminate these drawbacks while maintaining the excellent biological performance of natural bone.”
This search has led to the development of several alternatives:
- Allografts: Bone from human donors (typically cadavers)
- Xenografts: Bone derived from animal sources (typically bovine or porcine)
- Alloplasts: Synthetic bone substitute materials
While allografts and xenografts have their place in modern dentistry, they come with their own limitations, including potential disease transmission concerns, ethical considerations for some patients, and variable resorption rates.
This is where synthetic bone materials enter the picture—offering a safe, ethical, and increasingly effective alternative.
Understanding Synthetic Bone Materials: The Science Behind the Innovation
Synthetic bone graft materials (alloplasts) are laboratory-created substances designed to mimic the properties of natural bone. These materials have evolved dramatically over the past few decades, from simple space-maintaining substances to sophisticated biomaterials that actively promote bone regeneration.
Key Properties of Ideal Synthetic Bone Materials
According to research published in the Journal of Dental Research, the ideal synthetic bone material should possess:
- Biocompatibility: The ability to function in the body without causing adverse reactions
- Osteoconduction: Providing a scaffold for new bone growth
- Osteoinduction: Actively stimulating bone-forming cells
- Appropriate resorption rate: Breaking down as new bone forms
- Mechanical stability: Providing structural support during healing
- Ease of handling: Allowing convenient clinical application
- Cost-effectiveness: Making treatment accessible to more patients
Dr. Sarah Chen of Mayo Clinic explains: “The holy grail in synthetic bone materials is achieving the perfect balance between resorption and new bone formation. The material should disappear at precisely the rate that new bone forms—not too quickly, which could lead to collapse, and not too slowly, which could impede complete regeneration.”
Categories of Synthetic Bone Materials: A Comprehensive Overview
The field of synthetic bone materials has expanded dramatically, with several distinct categories now available for clinical use. Each offers unique properties and advantages for specific clinical situations.
1. Calcium Phosphate-Based Materials
Calcium phosphate compounds form the backbone of many synthetic bone materials due to their chemical similarity to the mineral phase of natural bone.
Hydroxyapatite (HA)
Composition: Ca₁₀(PO₄)₆(OH)₂ – the primary mineral component of natural bone
Key Properties:
- Excellent biocompatibility
- Outstanding osteoconductive properties
- Very slow resorption rate (sometimes considered non-resorbable)
- High compressive strength
Clinical Applications:
- Ridge preservation
- Sinus augmentation
- Periodontal defects
- Areas requiring long-term structural support
Limitations:
- Limited osteoinductive properties
- May remain visible on radiographs for years
- Can interfere with remodeling if complete resorption is desired
Beta-Tricalcium Phosphate (β-TCP)
Composition: Ca₃(PO₄)₂
Key Properties:
- Highly biocompatible
- Good osteoconductive properties
- Predictable resorption rate (typically 6-18 months)
- Porous structure allows for cell migration and vascularization
Clinical Applications:
- Extraction socket preservation
- Periodontal defects
- Cystic cavities
- Situations requiring complete replacement by natural bone
Limitations:
- Limited mechanical strength
- Resorption may occur too quickly in some clinical scenarios
- Minimal osteoinductive properties
Biphasic Calcium Phosphate (BCP)
Composition: Combination of hydroxyapatite and β-TCP in various ratios
Key Properties:
- Combines the stability of HA with the resorbability of β-TCP
- Customizable resorption rates based on the HA/β-TCP ratio
- Excellent osteoconductive properties
- Good handling characteristics
Clinical Applications:
- Versatile use in most bone augmentation procedures
- Particularly valuable in sinus lifts
- Implant site development
- Large defect reconstruction
Limitations:
- Variable performance based on specific formulation
- Limited osteoinductive properties without additives
A study published in the International Journal of Oral & Maxillofacial Implants found that biphasic materials with a 60/40 HA/β-TCP ratio showed optimal balance between stability and resorption for most dental applications.
2. Bioactive Glasses
Bioactive glasses represent a revolutionary category of synthetic bone materials that form direct chemical bonds with both bone and soft tissue.
Composition: Network of silicon dioxide with calcium oxide, sodium oxide, and phosphorus pentoxide
Key Properties:
- Forms a hydroxycarbonate apatite layer when exposed to biological fluids
- Creates strong chemical bonds with bone
- Stimulates osteoblast proliferation and differentiation
- Releases ions that promote bone formation
- Some formulations have antimicrobial properties
Clinical Applications:
- Periodontal defects
- Extraction socket preservation
- Ridge augmentation
- Particularly valuable in potentially contaminated sites due to antimicrobial properties
Limitations:
- Brittle nature limits use in load-bearing applications
- Variable resorption rates depending on specific formulation
- May cause transient inflammatory response in some patients
Dr. Robert Johnson, a researcher specializing in dental biomaterials, notes: “Bioactive glasses represent one of the most exciting advancements in synthetic bone materials. Their ability to form direct chemical bonds with bone and release therapeutic ions creates a dynamic healing environment that passive materials simply cannot match.”
3. Polymer-Based Bone Substitutes
Synthetic polymers offer unique advantages in bone regeneration, particularly in terms of customizability and controlled degradation.
Poly(lactic-co-glycolic acid) (PLGA)
Composition: Copolymer of lactic acid and glycolic acid
Key Properties:
- Biodegradable with controllable degradation rates
- Can be engineered into various forms (scaffolds, microspheres, etc.)
- Excellent carrier for growth factors and medications
- Minimal inflammatory response
Clinical Applications:
- Guided bone regeneration membranes
- Drug delivery systems for bone regeneration
- Composite materials with ceramic components
- Tissue engineering applications
Limitations:
- Limited mechanical strength
- Acidic degradation products can affect local pH
- Minimal osteoconductive properties without additives
Polycaprolactone (PCL)
Composition: Biodegradable polyester
Key Properties:
- Very slow degradation rate (2-4 years)
- Excellent processing capabilities (3D printing, electrospinning)
- Good mechanical properties
- Minimal inflammatory response
Clinical Applications:
- Long-term scaffolds for bone regeneration
- 3D-printed custom bone substitutes
- Composite materials with ceramic components
Limitations:
- Limited bioactivity without surface modifications
- Hydrophobic nature can limit cell attachment
- Slow degradation may be excessive for some applications
Research published in the Journal of Biomedical Materials Research highlights the potential of polymer-based materials in personalized medicine: “The ability to precisely control the architecture, degradation rate, and mechanical properties of polymer scaffolds makes them ideal candidates for patient-specific bone regeneration approaches.”
4. Composite Synthetic Materials
Recognizing that no single material possesses all the ideal characteristics, researchers have developed composite materials that combine the advantages of different components.
Polymer-Ceramic Composites
Composition: Combination of biodegradable polymers with ceramic particles (HA, β-TCP, bioactive glass)
Key Properties:
- Balanced mechanical properties (flexibility from polymers, strength from ceramics)
- Customizable degradation rates
- Enhanced biological activity compared to polymers alone
- Improved handling characteristics
Clinical Applications:
- Complex defect reconstruction
- Guided bone regeneration
- Custom 3D-printed bone substitutes
- Drug and growth factor delivery systems
Limitations:
- Manufacturing complexity
- Variable performance based on specific formulation
- Higher cost than single-component materials
Calcium Phosphate Cements (CPCs)
Composition: Powder and liquid components that set to form hydroxyapatite or brushite
Key Properties:
- Injectable and moldable
- Sets in situ (within the defect)
- Excellent defect filling capabilities
- Good biocompatibility and osteoconduction
Clinical Applications:
- Irregularly shaped defects
- Minimally invasive procedures
- Periodontal defects
- Extraction socket preservation
Limitations:
- Limited mechanical strength
- Setting reaction can generate heat
- Variable resorption rates depending on formulation
Dr. Lisa Rodriguez of the American Academy of Periodontology explains: “Composite materials represent the future of synthetic bone substitutes. By combining the best properties of different material classes, we can create solutions that more closely mimic the complex nature of natural bone.”
Advanced Innovations: Pushing the Boundaries of Synthetic Bone Materials
The field continues to evolve rapidly, with several cutting-edge approaches showing tremendous promise for the future of bone regeneration.
Growth Factor-Enhanced Synthetic Materials
By incorporating biological signaling molecules into synthetic scaffolds, researchers have created materials that actively promote bone formation.
Bone Morphogenetic Protein (BMP) Carriers
Innovation: Synthetic materials designed to release BMPs in a controlled manner
Advantages:
- Powerful osteoinductive properties
- Potential for faster bone regeneration
- May reduce the need for autogenous bone
Clinical Status:
- Some BMP-2 products are FDA-approved for specific dental applications
- Ongoing research focuses on optimizing delivery systems and dosages
Considerations:
- Higher cost than conventional materials
- Potential for adverse effects with high doses
- Regulatory considerations vary by country
Platelet-Rich Fibrin (PRF) Combined with Synthetics
Innovation: Patient’s own blood concentrates mixed with synthetic materials
Advantages:
- Enhances the biological activity of synthetic materials
- Introduces multiple growth factors naturally
- Improves handling properties
- Cost-effective approach to enhancing regeneration
Clinical Status:
- Widely used in clinical practice
- Growing body of evidence supporting efficacy
- Various protocols for preparation and application
Considerations:
- Results may vary based on patient factors
- Standardization challenges
- Requires blood draw and processing equipment
Nanotechnology in Synthetic Bone Materials
Manipulating materials at the nanoscale (1-100 nanometers) has opened new possibilities for mimicking the natural nanostructure of bone.
Nanostructured Calcium Phosphates
Innovation: Engineered at the nanoscale to mimic natural bone mineral
Advantages:
- Increased surface area for cell attachment
- Enhanced protein adsorption
- Improved mechanical properties
- More natural remodeling process
Clinical Status:
- Several products commercially available
- Growing clinical evidence base
- Continuing research on optimal nanostructures
Considerations:
- Manufacturing challenges
- Higher cost than conventional materials
- Long-term effects still being studied
Nanocomposite Materials
Innovation: Multiple materials combined at the nanoscale
Advantages:
- Unprecedented control over material properties
- Enhanced mechanical strength
- Customizable degradation profiles
- Potential for multiple therapeutic functions
Clinical Status:
- Primarily in research and development phase
- Some early clinical applications
- Rapid advancement expected in coming years
Considerations:
- Complex manufacturing processes
- Regulatory hurdles
- Cost considerations
A review in the Journal of Dental Research concluded: “Nanotechnology represents a paradigm shift in synthetic bone materials, allowing unprecedented control over material properties and biological interactions at the cellular level.”
3D-Printed Custom Bone Substitutes
The marriage of advanced imaging, computer-aided design, and additive manufacturing has revolutionized the potential for patient-specific bone regeneration.
Innovation: Custom-designed, 3D-printed scaffolds precisely matching the patient’s defect
Advantages:
- Perfect anatomical fit
- Optimized internal architecture for bone ingrowth
- Potential for incorporating multiple materials and biologics
- Reduced surgical time
Clinical Status:
- Emerging clinical applications
- Several case reports and small series published
- Regulatory pathways being established
Considerations:
- Equipment and expertise requirements
- Higher initial costs
- Longer preparation time
Dr. Michael Chen of Harvard School of Dental Medicine notes: “3D printing allows us to create not just the external shape of the defect but also to engineer the internal architecture of the graft. We can design specific porosity gradients and channels for vascularization that weren’t possible with traditional manufacturing methods.”
Clinical Applications: Matching the Material to the Challenge
Different clinical scenarios call for different synthetic bone materials. Understanding these applications helps both clinicians and patients make informed decisions.
Extraction Socket Preservation
Clinical Challenge: Preventing ridge collapse after tooth extraction
Ideal Material Properties:
- Easy handling in socket defects
- Appropriate resorption rate (3-6 months)
- Good space maintenance
- Support for soft tissue
Recommended Synthetic Options:
- β-TCP or biphasic calcium phosphate
- Bioactive glass particulates
- Composite materials with collagen
Evidence Base: Research published in the International Journal of Oral and Maxillofacial Surgery found that synthetic materials preserved an average of 85-90% of ridge dimensions compared to 40-60% with no grafting.
Sinus Lift Procedures
Clinical Challenge: Creating adequate bone volume in the posterior maxilla for implant placement
Ideal Material Properties:
- Excellent space maintenance
- Appropriate resorption rate (6-9 months)
- Good handling in the sinus environment
- Resistance to displacement during breathing
Recommended Synthetic Options:
- Biphasic calcium phosphate (higher HA content)
- Nanostructured calcium phosphates
- Composite materials with extended resorption profiles
Evidence Base: A systematic review in the Journal of Prosthodontics concluded that synthetic materials achieved comparable implant survival rates to other graft materials in sinus augmentation procedures.
Horizontal Ridge Augmentation
Clinical Challenge: Increasing the width of an atrophic alveolar ridge
Ideal Material Properties:
- Good stability under soft tissue pressure
- Appropriate resorption rate (6-12 months)
- Ability to support membrane placement
- Promotion of vascularization
Recommended Synthetic Options:
- Biphasic calcium phosphate blocks or granules
- Calcium phosphate cements with reinforcement
- Composite materials with enhanced mechanical properties
Evidence Base: Clinical studies have shown that synthetic materials can achieve 3-5mm of horizontal ridge gain when used with appropriate barrier membranes and fixation techniques.
Vertical Ridge Augmentation
Clinical Challenge: Increasing the height of the alveolar ridge (considered among the most challenging bone augmentation procedures)
Ideal Material Properties:
- Exceptional mechanical stability
- Controlled resorption rate
- Ability to support rigid membrane fixation
- Enhanced biological activity
Recommended Synthetic Options:
- Growth factor-enhanced composites
- Nanostructured materials with reinforcement
- Custom 3D-printed scaffolds
- Typically combined with autologous components
Evidence Base: While traditionally challenging with synthetic materials alone, newer composite approaches have shown promising results, with studies reporting 3-7mm vertical gain in selected cases.
Periodontal Regeneration
Clinical Challenge: Regenerating bone, cementum, and periodontal ligament in periodontal defects
Ideal Material Properties:
- Adaptability to irregular defect shapes
- Appropriate particle size for specific defects
- Controlled resorption rate
- Bioactivity to promote multiple tissue types
Recommended Synthetic Options:
- Bioactive glass particulates
- β-TCP or biphasic materials
- Growth factor-enhanced composites
- Nanomaterials with multiple biological functions
Evidence Base: Clinical trials have demonstrated that advanced synthetic materials can achieve comparable results to traditional approaches in periodontal regeneration, with some bioactive glass formulations showing particular promise in intrabony defects.
Patient Considerations: Making Informed Decisions
For patients like Sarah from our introduction, several factors should influence the decision regarding synthetic bone materials:
Advantages for Patients
- Elimination of donor site morbidity: No second surgical site means less pain and faster overall recovery.
- Unlimited availability: No concerns about limited autograft quantity, especially important for larger defects.
- Reduced surgical time: Typically results in shorter procedures and less time under anesthesia.
- Ethical and religious considerations: Synthetic materials address concerns some patients have about human or animal-derived products.
- Predictable properties: Manufactured under controlled conditions, synthetic materials offer consistent quality and performance.
Potential Limitations
- Cost considerations: Some advanced synthetic materials may be more expensive than traditional options, though this is often offset by reduced surgical time and elimination of donor site complications.
- Variable biological performance: While advancing rapidly, some synthetic materials may not yet match the biological activity of autografts in all situations.
- Learning curve for clinicians: Proper handling and application of synthetic materials requires specific training and experience.
- Specific contraindications: Some materials may not be suitable for patients with certain medical conditions or in the presence of active infection.
Dr. Wilson advises: “The conversation about graft materials should be a collaborative one between patient and clinician, considering not just the biological factors but also the patient’s preferences, values, and specific circumstances.”
Sarah’s Story: A Patient’s Perspective
Returning to Sarah from our introduction, after discussing the options, she chose a nanostructured biphasic calcium phosphate material for her bone augmentation procedure. Six months later, the site had developed sufficient bone volume for implant placement.
“I was initially skeptical about synthetic materials,” Sarah shared. “But the recovery was so much easier than I expected. Not having to deal with pain from a hip surgery while also recovering from the dental procedure made a huge difference. And the results speak for themselves—my implant is stable and feels completely natural.”
The Future of Synthetic Bone Materials: What’s on the Horizon
The field continues to evolve at a remarkable pace, with several exciting developments on the horizon:
Bioprinting of Bone Tissues
Beyond simple 3D printing of scaffolds, bioprinting involves the precise deposition of cells, growth factors, and materials to create living constructs.
Potential Impact: Could allow the creation of fully functional bone tissue in the laboratory, complete with vascularization and cellular components.
Timeline: Early clinical applications expected within 5-10 years.
Smart Materials with Responsive Properties
Materials that can respond to the local biological environment, changing their properties based on healing stage or mechanical demands.
Potential Impact: Could optimize the regeneration process by adapting to individual healing patterns and needs.
Timeline: Research advancing rapidly, with early clinical applications possible within 3-7 years.
Gene-Activated Matrices
Synthetic materials incorporating gene therapy approaches to stimulate specific cellular responses and protein production.
Potential Impact: Could provide highly targeted biological signals for enhanced regeneration with reduced side effects.
Timeline: Currently in preclinical development, with human trials likely within 5-8 years.
Integration with Digital Workflows
Seamless integration of intraoral scanning, CBCT imaging, treatment planning software, and manufacturing technologies.
Potential Impact: Will streamline the process from diagnosis to custom material fabrication, reducing treatment time and improving outcomes.
Timeline: Already beginning, with rapid advancement expected over the next 3-5 years.
Conclusion: The Transformative Impact of Synthetic Bone Materials
The evolution of synthetic bone materials represents one of the most significant advancements in modern dentistry. From simple space-maintaining substances to sophisticated biomimetic materials that actively promote regeneration, these innovations have transformed what’s possible in dental bone augmentation.
For patients like Sarah, synthetic bone materials offer a less invasive, more comfortable path to dental restoration. For clinicians, they provide versatile tools to address increasingly complex challenges. And for researchers, they represent a field of continuous innovation and discovery.
As Dr. Rodriguez concludes: “We’re witnessing a paradigm shift from simply replacing lost bone to regenerating functional tissue. The line between synthetic materials and biological tissues continues to blur, bringing us closer to true regenerative dentistry.”
Whether you’re a patient considering treatment options or a clinician evaluating materials for your practice, staying informed about these advances ensures you can benefit from the remarkable possibilities they offer.
Have you experienced a procedure using synthetic bone materials? We’d love to hear about your experience in the comments below.