Whitening Sensitivity: Causes and Solutions for Comfortable Treatment
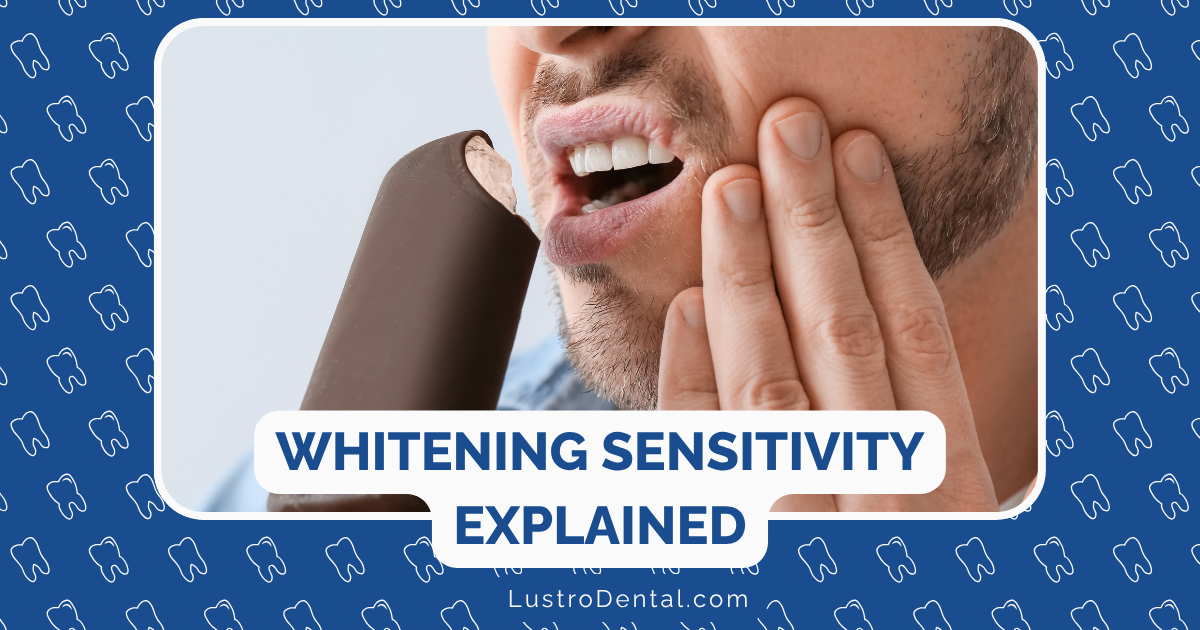
That sharp, shooting pain when you sip your morning coffee after a teeth whitening treatment isn’t just annoying—it’s enough to make you question whether that brighter smile was worth it. If you’ve experienced this, you’re not alone. Studies show that up to 80% of people experience some level of sensitivity during or after teeth whitening.
But here’s the good news: whitening sensitivity is both preventable and manageable. As someone who’s helped countless patients navigate this common side effect, I’m sharing everything you need to know about why sensitivity happens and how to enjoy your whitening journey with minimal discomfort.
Why Do Teeth Become Sensitive During Whitening?
Understanding the “why” behind whitening sensitivity helps us better address the problem. Here’s what’s actually happening in your mouth:
The Peroxide Effect
The active ingredient in most whitening products is either hydrogen peroxide or carbamide peroxide. While these ingredients are excellent at removing stains, they can temporarily irritate the nerve inside your tooth.
According to a 2023 study published in the Journal of the American Dental Association, peroxide molecules are small enough to penetrate through your enamel and dentin, reaching the pulp (where the nerve lives) in as little as 5-15 minutes. This direct contact with the nerve is what causes that zingy feeling.
Exposed Dentin Tubules
Your teeth contain thousands of microscopic channels called tubules that run from the surface through the dentin to the nerve. Whitening agents can temporarily open these tubules, making them more responsive to temperature changes, sweet foods, and even air.
Dr. Sarah Johnson of the American Academy of Cosmetic Dentistry explains: “Think of these tubules as tiny highways to your tooth’s nerve. Whitening temporarily widens these highways, allowing more stimuli to reach the nerve and trigger sensitivity.”
Concentration Matters
The higher the concentration of peroxide in your whitening product, the more likely you are to experience sensitivity. Professional in-office treatments, which may use concentrations of 25-40% hydrogen peroxide, typically cause more sensitivity than at-home options, which usually contain 3-15% hydrogen peroxide or 10-20% carbamide peroxide.
Who’s Most Likely to Experience Whitening Sensitivity?
Not everyone experiences the same level of sensitivity. You’re more likely to have significant discomfort if:
- You already have sensitive teeth
- You have receding gums that expose the roots of your teeth
- Your teeth have cracks or worn enamel
- You have existing dental work like fillings or crowns
- You’re using high-concentration whitening products
- You have a history of sensitive teeth after dental procedures
Prevention: Before You Whiten
The best approach to whitening sensitivity is preventing it before it starts. Here are proven strategies to minimize discomfort:
1. Start with a Dental Check-up
Before beginning any whitening treatment, visit your dentist to ensure your teeth are healthy. Cavities, cracks, or gum disease can significantly increase sensitivity and should be addressed first.
2. Use Desensitizing Toothpaste Before Treatment
Research published in the Journal of Clinical Dentistry shows that using toothpaste containing 5% potassium nitrate for two weeks before whitening can reduce sensitivity by up to 50%. Potassium nitrate works by blocking pain signals from the nerve, providing a protective barrier before you even start treatment.
Brands like Sensodyne or Colgate Sensitive Pro-Relief are excellent options. For maximum effectiveness, don’t rinse after brushing—this allows the active ingredients to continue working.
3. Consider Lower-Concentration Products
If you know you have sensitive teeth, start with a lower-concentration whitening product. According to the American Dental Association, products with 10% carbamide peroxide (equivalent to about 3.5% hydrogen peroxide) can still provide noticeable whitening with minimal sensitivity.
4. Take Anti-Inflammatory Medication
Taking an over-the-counter anti-inflammatory like ibuprofen about 30 minutes before your whitening treatment can help reduce inflammation and minimize sensitivity. A study from the University of Michigan found this approach particularly effective for in-office treatments.
During Treatment: Minimizing Discomfort
If you’re using at-home whitening products, these strategies can help reduce sensitivity during the process:
1. Shorten Treatment Time
Start with shorter application times than recommended—perhaps 15 minutes instead of 30—and gradually increase as your teeth adjust. This “low and slow” approach allows your teeth to acclimate to the whitening agent.
2. Reduce Frequency
Instead of daily treatments, try every other day or even twice a week. This gives your teeth time to recover between sessions.
3. Use Less Product
If you’re using trays, use only the recommended amount of gel. Excess gel can overflow onto gums, causing irritation, and won’t make your teeth whiter faster.
4. Choose Custom-Fit Trays
If possible, invest in custom-fit whitening trays from your dentist. These fit your teeth precisely, minimizing gel contact with gums and ensuring even application. According to the Journal of Esthetic and Restorative Dentistry, custom trays can reduce sensitivity by up to 30% compared to generic options.
After Whitening: Soothing Solutions
Even with the best prevention, you might still experience some sensitivity. Here’s how to address it:
1. Use Desensitizing Gel
Many dentists offer potassium nitrate desensitizing gels that can provide immediate relief. Research from a 2025 clinical trial found that higher concentrations of potassium nitrate (10% and 35%) were particularly effective at reducing both the prevalence and intensity of tooth sensitivity after professional whitening.
2. Apply Fluoride
Professional fluoride treatments containing 5% sodium fluoride can strengthen enamel and provide relief for up to eight weeks. At-home fluoride rinses can also help, though they’re less concentrated.
3. Adjust Your Diet
For 48-72 hours after whitening, avoid:
- Very hot or cold foods and beverages
- Acidic items like citrus fruits, tomatoes, and soda
- Sweet or sour foods
- Staining items like coffee, tea, and red wine
When drinking cold beverages, use a straw to minimize contact with your teeth.
4. Try Oil Pulling
Some patients find relief through oil pulling with coconut oil, which has natural anti-inflammatory properties. Swish a tablespoon of coconut oil in your mouth for 15-20 minutes, then spit it out (not down the drain, as it can solidify).
5. Salt Water Rinses for Gum Irritation
If your gums are irritated from the whitening process (appearing white or red), gentle salt water rinses can help reduce inflammation. Mix half a teaspoon of salt in 8 ounces of warm water and rinse several times daily.
When to See Your Dentist
While some sensitivity is normal, severe or prolonged pain isn’t. Contact your dentist if:
- Sensitivity lasts more than a week
- Pain is severe enough to disrupt sleep or daily activities
- Your gums become severely irritated or bleed
- You develop white spots on your teeth that don’t disappear within 48 hours
The Future of Sensitivity-Free Whitening
The good news is that dental researchers are continually working on ways to make whitening more comfortable. Recent innovations include:
- Calcium phosphate-containing whitening gels that help remineralize enamel during treatment
- LED-activated whitening systems that require lower peroxide concentrations
- Nanoparticle delivery systems that target stains more efficiently without penetrating deeply into the tooth
Finding Your Balance
Remember, teeth whitening doesn’t have to be an all-or-nothing approach. Finding the right balance between whitening effectiveness and comfort is key. As Dr. Michael Roberts, cosmetic dentistry specialist, notes: “The best whitening treatment is one that gives you results you’re happy with, at a sensitivity level you can tolerate.”
By understanding the causes of whitening sensitivity and implementing these prevention and treatment strategies, you can achieve that brighter smile without the ouch factor. Your future self—enjoying ice cream with your dazzling smile—will thank you.
Have you experienced sensitivity during teeth whitening? What solutions worked best for you? Share your experiences in the comments below!